Kidney int:中美洲肾病(Mesoamerican nephropathy)知多少?
2017-12-14 MedSci MedSci原创
中美洲肾病(Mesoamerican nephropathy)是一种病因不明的破坏性疾病,主要影响中美洲年轻的农业工人。目前,迫切需要了解该疾病的损伤机制和早期疾病进展过程,这将有助于确定疾病的根本原因,并进行针对性的直接治疗和预防工作。近期,一篇发表在杂志Kidney int上的文章前瞻性地描述了尼加拉瓜地区,急性患者发生最早临床表现时的中美洲肾病肾脏病理。研究者们考虑将血清肌酐、白细胞尿和白细
中美洲肾病(Mesoamerican nephropathy)是一种病因不明的破坏性疾病,主要影响中美洲年轻的农业工人。目前,迫切需要了解该疾病的损伤机制和早期疾病进展过程,这将有助于确定疾病的根本原因,并进行针对性的直接治疗和预防工作。
近期,一篇发表在杂志Kidney int上的文章前瞻性地描述了尼加拉瓜地区,急性患者发生最早临床表现时的中美洲肾病肾脏病理。
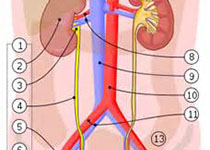
研究者们考虑将血清肌酐、白细胞尿和白细胞增多症或嗜中性粒细胞增多(或从基线至少增加0.3 mg/dL或1.5倍)纳入研究。通过超声引导的活组织检查获得肾组织,用于光、免疫荧光和电子显微镜检查。
结果显示,所有接受肾穿刺活检的11例患者均表现肾小管间质性肾炎,并伴有不同程度的炎症反应和慢性炎症。间质细胞浸润(主要是T淋巴细胞和单核细胞),且大部分在皮质髓质连接处;嗜中性粒细胞在管状腔内累积;肾小球基本保存;少量轻度的缺血性改变;并没有发现免疫沉积物。
肾小管间质性肾炎的急性成分为急性肾小管细胞损伤,间质水肿和早期纤维化。慢性肾小管间质性肾炎包括严重的管状萎缩,管状基底膜增厚和间质纤维化。对中美洲肾病的肾组织病理学研究揭示了原发性间质疾病伴有完整的肾小球的病理改变。
原始出处:
Fischer RSB, Vangala C, et al. Early detection of acute tubulointerstitial nephritis in the genesis of Mesoamerican nephropathy. Kidney Int. 2017 Nov 18. pii: S0085-2538(17)30726-3. doi: 10.1016/j.kint.2017.09.012.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#美洲#
26
#ESO#
27
#MES#
38
#kidney#
22
学习了.好文章
57