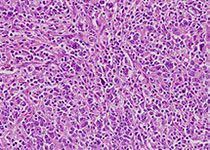
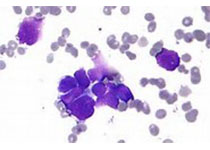
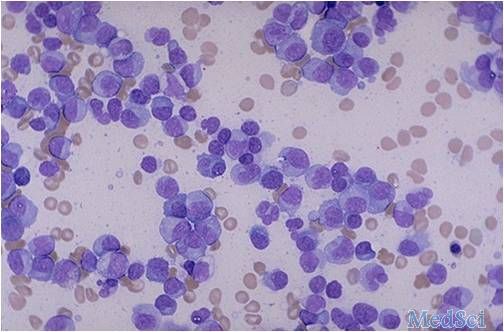
FDA加速批准acalabrutinib用于治疗套细胞淋巴瘤
2017-11-02 常路 环球医学
日前,美国食品和药物管理局(FDA)加速批准acalabrutinib用于治疗既往接受至少一次治疗的套细胞淋巴瘤成年患者。FDA药品评价和研究中心Richard Pazdur博士表示,套细胞淋巴瘤是一种特别具有侵袭性的癌症。对于对治疗无响应或复发的患者,acalabrutinib提供了一种新的治疗方案,在初步研究中该药物对一些患者已经显示出高响应率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#细胞淋巴瘤#
37
#ALA#
39
#ACA#
28
#acalabrutinib#
32
vvcxxbbbvcvghb
60