HAEMATOLOGICA:口服阿扎胞苷为缓解期急性髓系白血病患者保持良好的疲劳水平和健康相关的生活质量
2021-12-21 MedSci原创 MedSci原创
对于缓解期的 AML 患者,健康相关生活质量 (HRQoL) 和疲劳通常会随着时间的推移而改善;理想的维持治疗应在不影响 HRQoL 的情况下延长生存期。
尽管强化化疗 (IC) 的缓解率相对较高,但大多数急性髓系白血病 (AML) 患者会复发,并且复发 AML 的总生存率 (OS) 令人沮丧。对于缓解期的 AML 患者,健康相关生活质量 (HRQoL) 和疲劳通常会随着时间的推移而改善;理想的维持治疗应在不影响 HRQoL 的情况下延长生存期。
此处报道一研究团队QUAZAR AML-001试验的结果,QUAZAR AML-001 是一项随机、双盲、安慰剂对照的 III 期试验。研究设计和终点在别处详细报告*(Wei A, Dohner H, Pocock C. Oral azacitidine maintenance for acute myeloid leukemia in first remission. N Engl J Med. 2020; 383(26):2526-2537. )。
简而言之,年龄≥55 岁、诊断时具有中危或低危细胞遗传学、ECOG PS ≤3 且不适合移植的患者随机接受口服 AZA 300 mg 或安慰剂,每天一次,共 14 天/28 天在达到首次 CR 或 CR 后 4 个月内循环,血液学恢复不完全(CRi)和 IC(诱导 ± 巩固)。在研究中以 5-15% 原始细胞复发的患者可以根据治疗研究人员的判断接受递增的 21 天/周期给药方案。
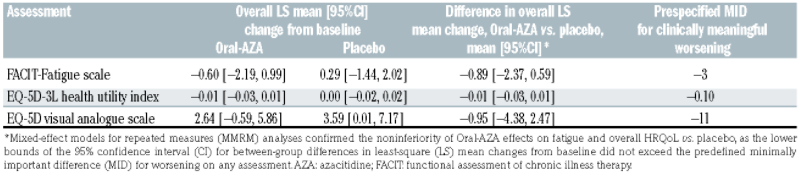
表 1:用于重复测量分析的混合效应模型:每组内相对于基线的总体最小二乘均值变化、总体最小二乘法均值变化的组间差异以及每次评估的预先指定的最小重要差异。
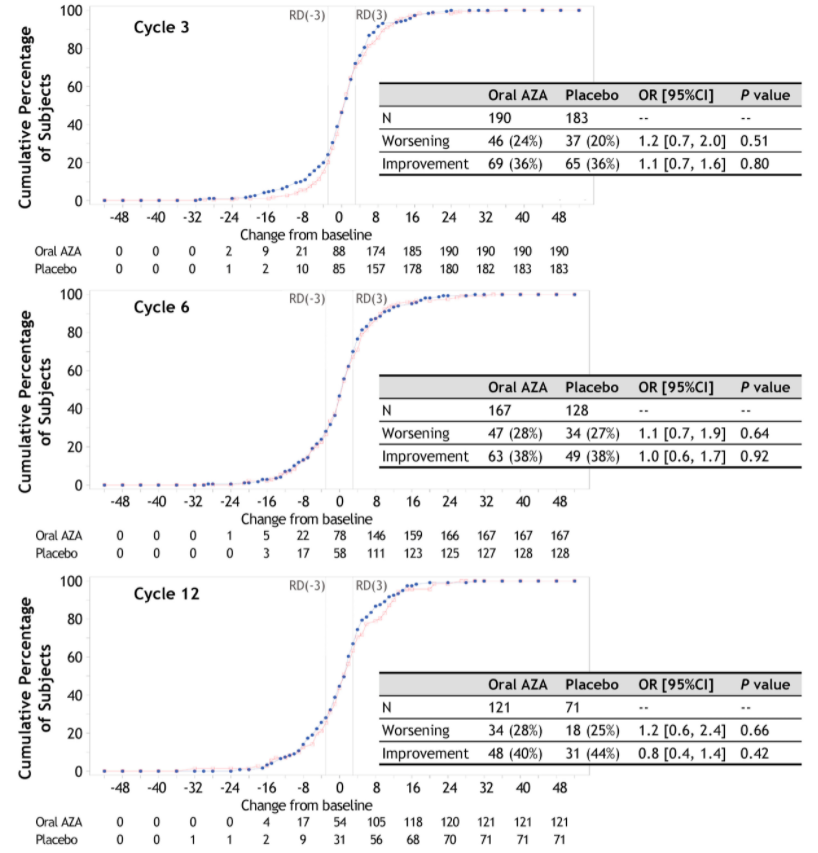

图 1:口服阿扎胞苷和安慰剂组个体患者在第 3、6、12 和 24 周期观察到的 FACIT-疲劳评分从基线变化的经验累积分布频率曲线。正变化评分包括从基线的改善。基线变化≥3 用于定义有临床意义的改善和恶化。优势比、95% 置信区间 (CI) 和P值使用 Cochran-Mantel-Haenszel 检验估计,通过随机分层因素进行分层。ECDF:经验累积分布频率;AZA:阿扎胞苷;FACIT:慢性病治疗的功能评估;RD:响应者定义。
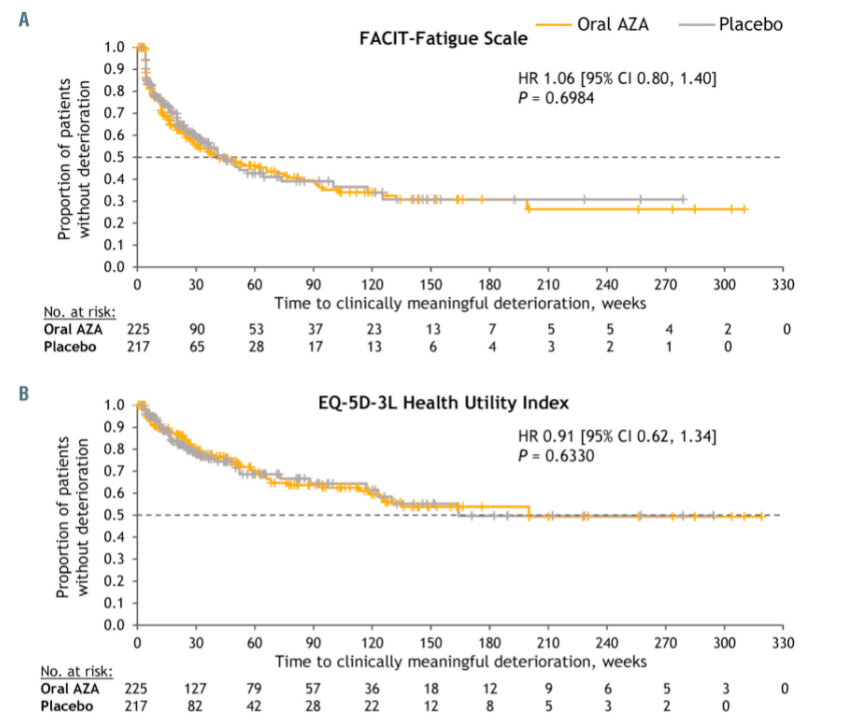

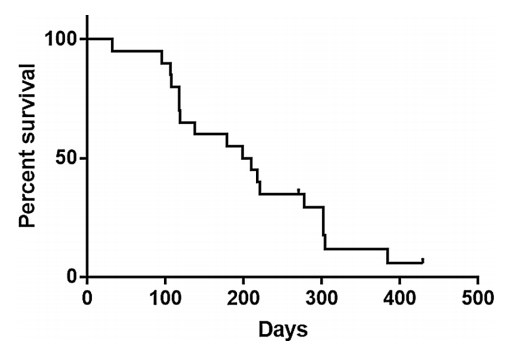
图 2: Kaplan-Meier 从基线到确认恶化的估计时间。(A) FACIT-疲劳量表。(B) EQ-5D-3L 健康效用指数。(C) EQ-5D 视觉模拟量表分数。明确恶化的时间定义为从随机化到连续≥2 次评估访问持续有临床意义恶化的时间。cAZA:阿扎胞苷;FACIT:慢性病治疗的功能评估;CI:置信区间;HR:风险比。
如前所述,在任何基线后访问中,治疗组内或口服 AZA 和安慰剂组之间观察到的从基线 FACIT-疲劳或 EQ-5D-3L HUI 评分的平均变化没有临床意义的差异。
eCDF 曲线详细说明了口服 AZA 和安慰剂组在第 3、6、12 和 24 周期中个体 FACIT-疲劳变化自基线的变化,通常重叠,每次就诊时报告有临床意义的改善或恶化的患者比例相似(图 1)。在两个治疗组中,每项措施具有临床意义恶化的患者比例都很低,并且在几乎所有基线后访问中,每种仪器上各组之间的比率相似(在线补充图 S1); Oral-AZA 组在第 19 个周期(EQ-5D VAS)和第 29 个周期(FACIT-疲劳)的恶化率显着更高,但这些可能是偶然发生的,因为这些分析不包括对多次测试的任何调整。Oral-AZA 组和安慰剂组在每种仪器上确认恶化的时间相似。在 FACITFatigue 上,Oral-AZA 的估计确认恶化的中位时间为 41 周,安慰剂为 44 周(风险比 [HR]:1.06;95% CI:0.80-1.40);EQ-5D-3L HUI 分别为 200 和 164 周(HR:0.91;95% CI:0.62-1.34);与EQ-5D VAS 的 136 周相比未达到(HR:0.86;95% CI:0.61-1.22)。在对死亡时的患者进行审查时观察到类似的发现。
虽然提高生存率是 AML 治疗的主要目标,但系统评估治疗对 HRQoL 的影响至关重要,因为如果伴随着与药物相关的 HRQoL 下降,延长生存期可能意义不大。QUAZAR AML-001 是首个前瞻性研究长期维持治疗对 IC 后缓解的 AML 患者 HRQoL 影响的安慰剂对照研究。在研究开始时,这些老年患者(中位年龄 68 岁)报告的疲劳水平和总体 HRQoL 总体良好,与一般人群的水平相当。在几乎所有的基线后评估中,口服 AZA 治疗期间的平均 FACIT-疲劳和 EQ-5D-3L 评分保持在或高于基线水平,纵向 MMRM 分析证实了口服 AZA 相对于安慰剂在保持 HRQoL 方面的非劣效性。这些 HRQoL 数据也与 QUAZAR AML-001 中 Oral-AZA 报告的可控安全性和可接受的耐受性一致。
这项研究的限制是 HRQoL 评估是在每个 28 天治疗周期的第 1 天进行的,允许在每个 14 天给药期后恢复 14 天。此外,与 AML 缓解期间的“仅观察”方法相比,两组患者都必须接受常规医院就诊、检测和骨髓采集,这可能会对 HRQoL 结果产生负面影响。
总的来说,口服 AZA 给药提供了许多潜在的好处,包括对患者的最佳便利性、无注射部位反应、更少的就诊次数和更低的相关成本,以及长期使用的治疗灵活性。QUAZAR AML-001 的结果表明,Oral-AZA 可显着改善 OS 和 RFS,而不会影响缓解期 AML 患者的疲劳或整体 HRQoL。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#HAE#
45
#缓解期#
37
#髓系白血病#
48
首次评论
45
👍非常好
55
#疲劳#
44
#EMA#
28