Clin Cancer Res:西妥昔单抗+纳武单抗联合治疗复发/转移性头颈部鳞癌
2022-04-07 xiaozeng MedSci原创
西妥昔单抗与纳武单抗的联合方案在复发性/转移性头颈部鳞状细胞癌中展现出了一定的治疗活性,值得进一步研究
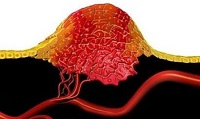
美国每年新增约6.7万例头颈部鳞状细胞癌(HNSCC)。头颈部鳞状细胞癌的主要风险因素有吸烟、酗酒和人乳头状瘤病毒(HPV)感染。初诊患者的预后一般较好,HPV相关患者的3年总生存率超过90%,非HPV相关患者的3年总生产率低于50%。但是,患者一旦发生复发或转移,就难以治愈。
这是一项多机构的2期临床试验,旨在明确复发性/转移性(R/M)头颈部鳞状细胞癌(HNSCC)患者采用西妥昔单抗联合纳武单抗治疗的总生存率(OS)。
招募了复发性/转移性头颈部鳞状细胞癌患者,予以西妥昔单抗(500 mg/m2)+纳武单抗(240 mg)治疗24个疗程。主要终点是一年总生存率(OS)。此外,研究人员还分析了收集到的肿瘤组织中p16和PD-L1的表达水平,以及血浆中HPV的DNA载量。
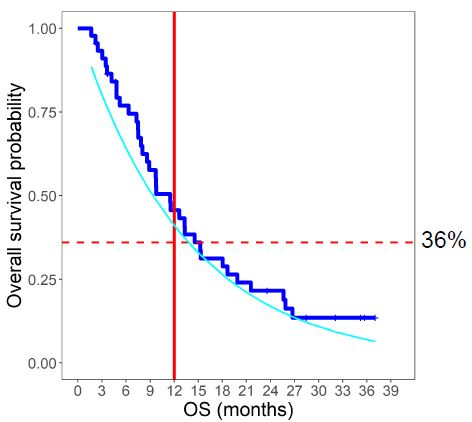
A队列和B队列的总生存率
共招募了95位患者,其中88位被纳入总生存期分析,并根据既往有无治疗过分成两个队列:A队列(n=45),既往接受过针对R/M HNSCC的治疗;B队列(n=43),既往未接受过相关治疗。中位随访了15.9个月,A队列的中位总生存期是11.4个月,一年总生存率是50%。B队列的中位总生存期是20.2个月,一年总生存率是66%。
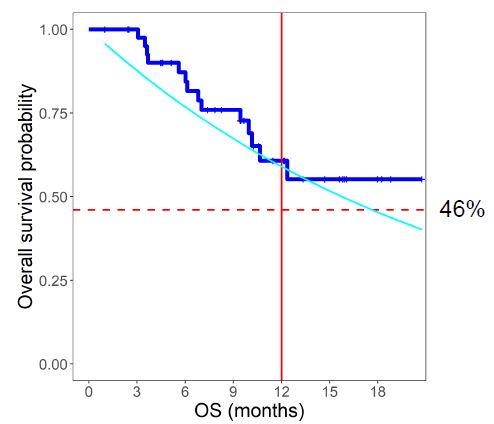
根据p16状态分组的无进展生存率
在总队列中,p16阴性与更高的缓解率相关(p=0.02),但对生存期无明显影响;较高的PD-L1联合阳性评分与高缓解率(p=0.03)和更长的总生存期(p=0.04)相关。在p16阳性的患者中,与HPV DNA载量较高的患者相比,HPV DNA计数低于更高的缓解率(p=0.01)和更长的总生存期(p=0.05)相关。
根据HPV DNA水平分组的总生存率
该研究显示,无论是在既往接受过治疗的还是未接受过治疗的复发性/转移性头颈部鳞状细胞癌中,西妥昔单抗与纳武单抗的联合方案都展现出了一定的治疗活性,值得进一步研究。
原始出处:
Chung Christine H,Li Jiannong,Steuer Conor E et al. Phase II multi-institutional clinical trial result of concurrent cetuximab and nivolumab in recurrent and/or metastatic head and neck squamous cell carcinoma.[J] .Clin Cancer Res, 2022, https://doi.org/10.1158/1078-0432.CCR-21-3849
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#西妥昔#
38
#联合治疗#
56
#转移性#
30
#鳞癌#
40
#头颈部#
36
#颈部#
38