Clin Cancer Res:托瑞帕利单抗二线治疗转移性尿路上皮癌的疗效、安全性和生物标志物
2021-11-10 Nebula MedSci原创
托瑞帕利单抗用作一线治疗失败的转移性尿路上皮癌患者的二线疗法展现出了令人鼓舞的临床活性,而且具有可控的安全性
免疫疗法为经标准治疗失败的转移性尿路上皮癌 (mUC) 患者提供了二线选择,但预测 mUC 患者对免疫治疗反应的生物标志物仍有待探索。
本研究旨在评估托瑞帕利单抗(toripalimab)在既往接受过治疗的 mUC 患者中的安全性、有效性和相关生物标志物。
招募的 mUC 患者接受托瑞帕利单抗 3 mg/kg Q2W 治疗。独立的审查委员会每 8 周评估一次临床反应(RECIST v1.1)。同时检测患者肿瘤 PD-L1 的表达、肿瘤突变负荷(TMB)和其他生物标志物。
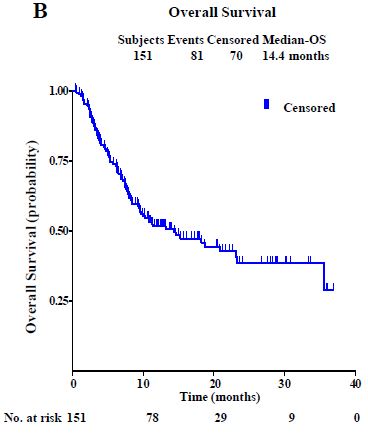
意向治疗人群的总生存率
在意向治疗人群(n=151)中。85%的患者经历过治疗相关的副反应(TRAE),20%的患者经历过3级或更严重的 TRAE。客观缓解率(ORR)为26%,疾病控制率(DCR)为45%。中位缓解持续时间、无进展生存期(PFS)和总生存期(OS)分别是19.7个月(95% CI 13.9-未达到)、2.3个月(1.8-3.6)和14.4个月(9.3-23.1)。
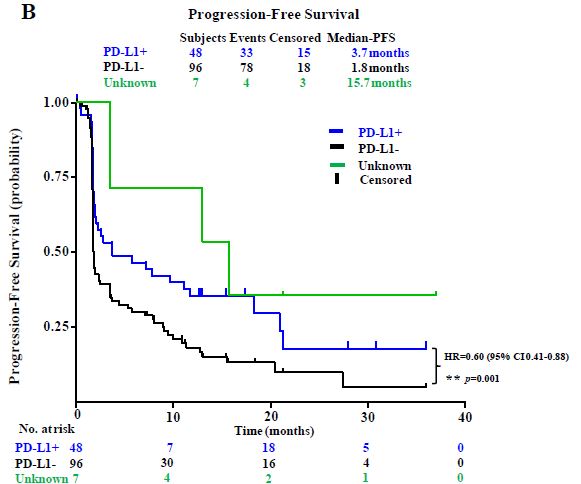
PD-L1 阳性或阴性患者的无进展生存率
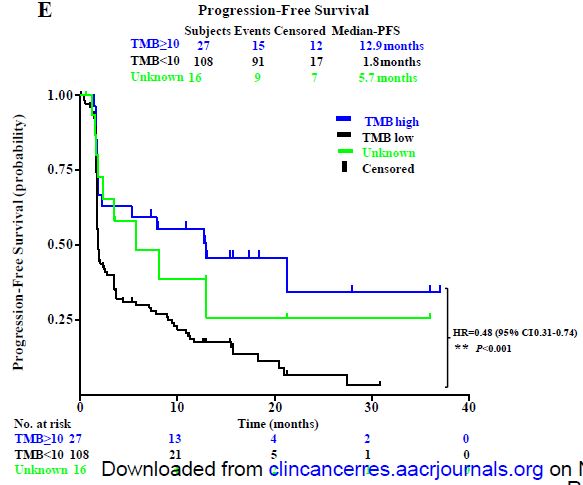
PD-L1 阳性和高 TMB 值(≥10个突变/Mb)的患者的客观缓解率明显高于 PD-L1 阴性患者(42% vs 17%;p=0.002)和低 TMB 值患者(48% vs 22%;p=0.014)。高 TMB 值组患者还表现出较低 TMB 值组更好的 PFS(12.9 vs 1.8个月;p<0.001)和 OS(未达到 vs 10.0个月;p=0.018)。
高TMB值和低TMB值患者的无进展生产率
总而言之,该研究结果表明,托瑞帕利单抗用作一线治疗失败的转移性尿路上皮癌患者的二线疗法展现出了令人鼓舞的临床活性,而且具有可控的安全性。PD-L1 和 TMB 值可作为预测患者对免疫治疗反应性的两个独立的生物标志物。
原始出处:
Sheng Xinan,Chen Haige,Hu Bin et al. Safety, Efficacy and Biomarker Analysis of Toripalimab in Patients with Previously Treated Advanced Urothelial Carcinoma: Results from a Multicenter Phase II Trial POLARIS-03.[J] .Clin Cancer Res, 2021, https://doi.org/10.1158/1078-0432.CCR-21-2210
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标志物#
24
#转移性#
39
#转移性尿路上皮癌#
33
#上皮癌#
42
#二线治疗#
36
#生物标志#
29
#生物标志#
30
👍👍👍
58
感谢老师,非常实用,学习了。。。。。
56
已读已读已读已读已读已读已读已读已读已读已读已读已读已读
0