JAMA oncology:晚期非小细胞肺癌局部放疗,生存期延长近3倍
2018-06-26 肿瘤 肿瘤
2017年9月,权威肿瘤学杂志《JAMA oncology》发表了一项重磅的2期临床试验结果:晚期非小细胞肺癌,在接受了4-6个疗程的化疗后,肿瘤缓解或者稳定的情况下,对残余的病灶进行立体定向放疗(SABR),可以将生存期提高近3倍!这是一项单中心的随机II期研究,入组条件是接受较为猛烈的双药化疗4-6个疗程后,疾病未出现进展的患者。一共入组了29名患者,分成2组。一组接受单药、靶向药等温和的全身
2017年9月,权威肿瘤学杂志《JAMA oncology》发表了一项重磅的2期临床试验结果:晚期非小细胞肺癌,在接受了4-6个疗程的化疗后,肿瘤缓解或者稳定的情况下,对残余的病灶进行立体定向放疗(SABR),可以将生存期提高近3倍!
这是一项单中心的随机II期研究,入组条件是接受较为猛烈的双药化疗4-6个疗程后,疾病未出现进展的患者。一共入组了29名患者,分成2组。一组接受单药、靶向药等温和的全身治疗维持;另外一组先对残余的病灶做立体定向放疗,然后再接受温和的全身治疗维持。
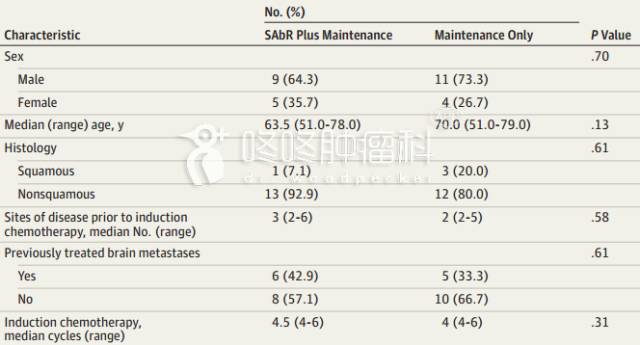
两组患者的性别、年龄、病理类型、转移灶的数目、脑转移情况以及入组前接受的化疗疗程数,无统计学差异。
这项研究本来计划入组36名患者,结果刚刚入组完29名患者,独立的疗效评审委员会就叫停了试验,因为明显加入放疗的这一组的生存期碾压式的好。胜负已经很明显了,比赛提前终止。
那么,到底是个什么样的比赛结果呢?
从2014年4月到2016年7月,入组病人、接受治疗并且完成随访,每一位病友的中位随访时间为9.6个月。诱导化疗最长用的方案是培美曲塞+卡铂(48%),维持治疗药物最常用的是单药培美曲塞(62%)。接受局部治疗的那一组,所有病人的所有病灶均接受了放疗,14例患者的31处病灶接受了放疗。
两组未发生治疗副作用导致的死亡,两组3-4级副作用发生情况类似。
两组的无疾病进展生存期,分别为9.7个月和3.5个月——局部放疗的加入,让生存期延长了近3倍!
更为重要的是:未接受放疗的15位病友中,有10位已经出现了疾病进展,其中7位就表现为原有病灶的进展;而接受过放疗的14位病友,无1例出现原有病灶的进展;也就是说,对原有残余病灶的放疗,至少很大程度上遏制了这些病灶的进一步进展和复发。

当然,上述研究仅纳入了29位患者,同时每一位患者接受的诱导化疗和巩固化疗的方案也不统一,还存在较大瑕疵。目前,设计更严谨、规模更大的三期临床试验,正在招募志愿者。
参考文献:
Consolidative Radiotherapy for Limited Metastatic Non-Small-Cell Lung Cancer: A Phase 2 Randomized Clinical Trial. JAMA Oncol. 2017 Sep 24:e173501. doi: 10.1001/jamaoncol.2017.3501
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncology#
26
#Oncol#
29
#非小细胞#
26
#生存期#
27
#局部#
0
谢谢分享.学习了
43
不错
64
学习谢谢分享
54
学习
39