Eur Radiol: 放射组学——如何能深度挖掘系统性硬化症相关间质性肺病HRCT图像信息
2021-02-18 shaosai MedSci原创
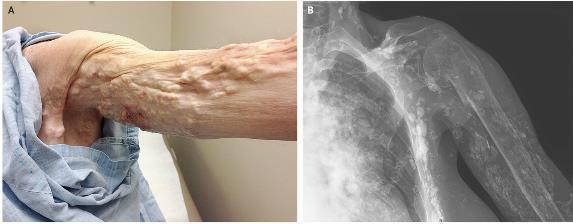
间质性肺疾病(ILD)是系统性硬化症(SSc)常见的并发症,同时是SSc相关死亡的主要原因。早期诊断SSc-ILD对临床治疗和患者预后具有重要的意义。
间质性肺疾病(ILD)是系统性硬化症(SSc)常见的并发症,同时是SSc相关死亡的主要原因。早期诊断SSc-ILD对临床治疗和患者预后具有重要的意义。新的成像方法如定量计算机断层扫描(CT)、磁共振成像(MRI)和核成像已被应用于ILD的诊断,以提供预后、功能和代谢等方面信息。到目前为止,高分辨率CT (HRCT)作为一种无创、经济且敏感的技术,能够在临床前阶段发现肺组织病理改变并进行预后评价,是诊断ILD的金标准。
放射组学是影像学图像向高维数据的转换,是一个新兴的技术研究领域。特征提取是放射组学的关键步骤,包括从预定义的感兴趣区域(ROI)计算纹理、密度和形状。放射组学具有对组织特征进行客观量化的优势,并能够检测常规视觉分析无法描述的影像学图像中的异常。
近日,发表在European Radiology杂志的一项研究回顾性使用基于纹理分析的放射组学特征和单纯的高分辨率计算机断层扫描(HRCT)视觉分析两种方法检测系统性硬化症(SSc)患者间质性肺疾病(ILD)的存在并对疾病进行分期,评价了两种方法诊断性能的差异,为临床提供一个更准确且敏感的早期诊断SSc-ILD的影像学方法。

本研究回顾性分析了60例(女性46例,中位年龄56岁)行胸部HRCT检查的SSc患者。由两名放射科医师进行视觉分析,以确定是否存在ILD特征。根据临床资料(性别、年龄、肺功能试验)计算性别、年龄和肺功能(GAP)分期。进行数据扩充,并将平衡数据集分为训练数据集(70%)和测试数据集(30%)。使用Akaike信息准则(AIC)拟合并比较了单、多逻辑回归模型对GAP阶段分类变量的选择。通过受试者工作特征(ROC)分析的曲线下面积(AUC)来评价诊断准确性,并计算诊断的敏感性和特异性。
与GAP1患者相比,GAP2患者的某些放射组学特征值显着降低(p <0.05),而其他放射学特征值显着升高(p = 0.001)。在多变量模型中两个特定放射组学特征的组合导致最低AIC为10.73,AUC为0.96,灵敏性为84%,特异性为99%。在预测个体GAP分期时,纤维化的视觉评估较差(AUC 0.86;敏感性83%;特异性74%)。

图 箱线图显示了GAP1和GAP2患者在多步降维和特征选择过程中提取出的6个最重要的放射组学特征之间的差异
放射组学与GAP分期具有相关性,但与ILD-HRCT的可视特征无关,这表明放射组学或许可在HRCT图像上提取到无法通过视觉分析识别的提示SSc-ILD严重程度的特征。本研究中建立的基于纹理分析的放射组学特征将为其进一步成为计算机辅助影像学决策的有价值的工具提供了理论上的支持和验证。
原始出处:
K Martini,B Baessler,M Bogowicz,et al. Applicability of radiomics in interstitial lung disease associated with systemic sclerosis: proof of concept.DOI:10.1007/s00330-020-07293-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#系统性#
31
#间质性肺病#与#人工智能#
0
#肺病#
31
#间质性#
33
#硬化症#
31
#系统性硬化#
27
哇哦
81