J Clin Oncol:前瞻性评估液体活检技术在针对不同耐药机制的转移性前列腺癌的临床预后作用
2021-07-03 yd2015 MedSci原创
研究证明,液体活检对肿瘤循环细胞(CTCs)中检测到的转录谱可以作为转移性前列腺癌患者中AR-V7以外的独立预后标志物。
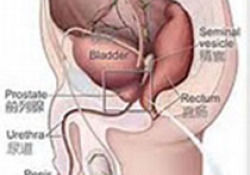
雄激素受体(AR)信号抑制剂(ARSIs),包括醋酸阿比特龙(AA)、恩杂鲁胺(enzalutamide)、apalutamide和darolutamide,可以改善男性转移性去势敏感前列腺癌(CSPC)和去势耐受前列腺癌(CRPC)的生存期。然而,大约5%-10%的患者将对ARSI治疗产生原发耐药性,并且大多数初始应答者将在1-3年内产生耐药性。多样化的耐药机制包括AR通路的结构性激活,由AR基因组结构改变、AR剪接变异(AR vs)的表达、AR依赖的丧失和神经内分泌前列腺癌的可塑性驱动。了解这些耐药机制有组于优化治疗。因此,国外学者采用一种新的液体活检技术从循环肿瘤细胞(CTCs)中收集mRNA,以检测AR- vs、AR靶点和神经内分泌前列腺癌(NEPC)标志物的表达,从而研究其在临床预后的作用。相关成果发表在Journal of Clinical Oncology杂志上。
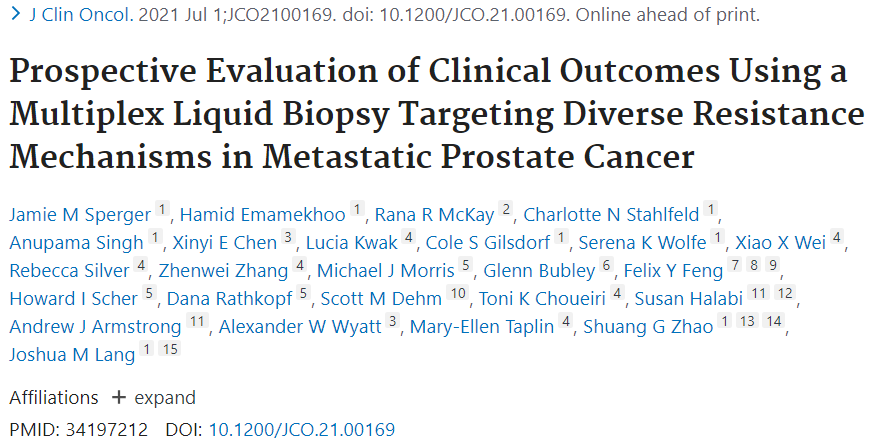
其中99例患者作为实验集,2项前瞻性II期临床研究的患者作为验证集(NCT01942837 [N=21] 和NCT02025010 [N =27])。包括CSPC (28%), CRPC (67%),和NEPC (6%)。根据CTC中AR等相关基因表达鉴别为两组显著的数据集(Cluster 1和2)。Cluster1(C1)的特征是AR调节的基因表达减少或缺失。C1包括所有组织学诊断为NEPC的患者。相反,Cluster2 (C2)在AR转录靶点高表达的患者中富集,表明AR转录活性增加。与AR活性增加相一致,C2组患者的血清PSA水平(中位数216 ng/mL)高于第1组患者(中位数11.22 ng/mL, P<0.0001)。
C1和C2的特征
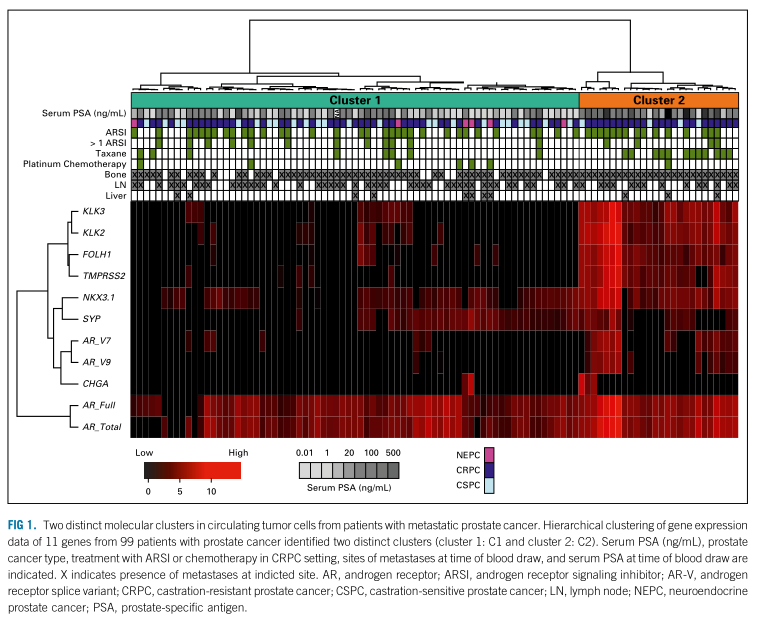
C2和C1组患者的中位OS分别为8.6个月(95% CI, 2.6 to 12.6) (n=26) 和 22.4个月 (95% CI, 12.5 to 34.9) (n =73) (P <0 .01, [HR]=3.45,95%CI,1.91 to 6.21)。AR-V+患者 (AR-V7 和AR-V9)和AR-V-患者 的中位OS为8.6个月(95% CI, 3.9 to 14.6) (n=24)和19.1 (95% CI, 12.3 to 30) (n=75) for AR-V– (P <0.01, HR=2.49,95%CI 1.39 to 4.47)。
OS
在多变量分析(MVA)中,在调整患者年龄、CRPC与CSPC、NEPC与CSPC、PSA、内脏转移和AR-状态后,C2是较短的OS独立预后因素。CRPC和NEPC是其他变量中跟OS有关的独立预后因素。

预后因素
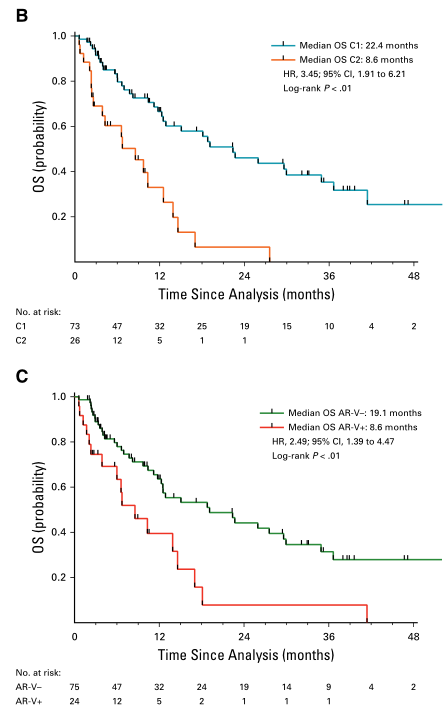
两项临床研究共48例患者作为验证集,其中10例患者被鉴定为Cluster2 (C2)。C2和C1组的中位OS分别15.2个月 [95% CI, 4.4 to未达到 (NR)]和未达到(P<0.01; HR=8.43,95%CI 2.74 to 25.92)。C2组患者较C1组患者的前列腺特异性抗原无进展生存期(PSA-PFS)明显缩短(3.6个月 [95% CI, 1.7 to NR] v 12个月[95% CI, 5.6 to 14]; P<0.01,HR=4.64 [1.53 to14.11])。同样C2组患者的影像学无进展生存期(rPFS)较短(2.7个月 [95% CI, 1 to NR] v 40.6个月[95% CI, 11 to NR]; P<0.01; HR=5.63 [1.82 to 17.41])。
验证集评估C1和C2的预后
综上,研究证明,液体活检对肿瘤循环细胞(CTCs)中检测到的转录谱可以作为转移性前列腺癌患者中AR-V7以外的独立预后标志物,并可用于识别多种ARSI耐药机制的出现。目前正在其他前瞻性试验中对此进行研究。
原始出处:
Sperger JM, Emamekhoo H, McKay RR, et al. Prospective Evaluation of Clinical Outcomes Using a Multiplex Liquid Biopsy Targeting Diverse Resistance Mechanisms in Metastatic Prostate Cancer. J Clin Oncol. 2021 Jul 1:JCO2100169. doi: 10.1200/JCO.21.00169. Epub ahead of print. PMID: 34197212.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#前瞻性#
37
#耐药机制#
32
#液体活检技术#
41
#Oncol#
28
#活检#
35
#转移性#
22
#转移性前列腺癌#
36
#临床预后#
30
谢谢梅斯分享这么多精彩信息
47
机制研究离临床仍然有距离,不过与临床结合思考,仍然有帮助的,不能仅仅是纯临床思维,转化思维同样重要
60