Clin Cancer Res:HER2+早期乳腺癌新辅助曲妥珠单抗后pCR取决于HER2/CEP17比值
2017-07-26 Aries 肿瘤资讯
既往研究表明HER2+及三阴性乳腺癌患者在新辅助化疗后更容易获得病理完全缓解,曲妥珠单抗的出现改善了HER2+乳腺癌患者的生存预后以及新辅助治疗的效果。那到底哪些HER2+的患者对新辅助靶向治疗的效果更佳呢?奥利地一篇前瞻性研究有了新的发现并发表在《Clinical Cancer Research》。 目的:本研究旨在探究新辅助曲妥珠单抗治疗后病理完全缓解率(pCR)是否取决于H
既往研究表明HER2+及三阴性乳腺癌患者在新辅助化疗后更容易获得病理完全缓解,曲妥珠单抗的出现改善了HER2+乳腺癌患者的生存预后以及新辅助治疗的效果。那到底哪些HER2+的患者对新辅助靶向治疗的效果更佳呢?奥利地一篇前瞻性研究有了新的发现并发表在《Clinical Cancer Research》。
目的:本研究旨在探究新辅助曲妥珠单抗治疗后病理完全缓解率(pCR)是否取决于HER2扩增水平。
方法:纳入114名HER2过表达并接受新辅助曲妥珠单抗的早期乳腺癌患者。ISH评估HER2及第17对染色体中心粒(CEP17)扩增情况并分析HER2/CEP17比值与pCR的关系。
结果:ypT0N0:HER2/CEP17>6(高水平扩增) vs. HER2/CEP17≤6分别为69.0%vs.30.4%(p=0.001)。ypT0/isN0或ypTis: HER2/CEP17>6(高水平扩增)vs. HER2/CEP17≤6分别为69.0%vs.30.4%(p=0.001) 75.9%和82.8%vs.39.1%和38.3%(p=0.002和P<0.001)。Logistic回归分析显示高水平的HER2扩增是唯一与pCR相关的因素,并且这种相关性几乎仅限于HR+乳腺癌。
结论:治疗前肿瘤穿刺病理HER2/CEP17>6与高pCR率显着相关,特别是对于HR+HER2+乳腺癌患者,HER2/CEP17比值可成为预测治疗反应的生物标记物。
介绍
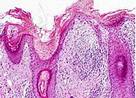
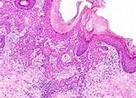
约18-20%乳腺癌出现HER2扩增。目前检测HER2扩增包括免疫组织化学法(IHC)及原位杂交法(ISH)。前者检测细胞表面HER2蛋白表达水平并得到0-3+的半定量评分,3+提示HER2+。ISH法检测第17个染色体上HER2基因拷贝数以及第17个中心粒拷贝数。根据ASCO/CAP临床实践指南,HER2/CEP17比值>2或HER2拷贝数绝对值>6视为HER2扩增。我们前期研究结果显示HER2+转移性乳腺癌患者中HER2/CEP17>6提示进展更快但对曲妥珠单抗的治疗反应率更高,PFS改善。基于此,我们假设治疗前HER2/CEP17>6的HER2+乳腺癌患者在新辅助曲妥珠单抗治疗后更容易获得pCR。
方法
本研究属于ABCSG转化科研项目的一部分。患者随机分配到前瞻性新辅助研究ABCSG-24和32。对于前者,HER2+浸润性乳腺癌患者随机分配到新辅助表柔比星/多西他赛q3w±卡培他滨加或不加曲妥珠单抗组。对于后者,HER2+乳腺癌患者按1:1:1:1随机分配到多西他赛+曲妥珠单抗组;多西他赛+贝伐单抗+曲妥珠单抗组;多西他赛+脂质体多柔吡星+曲妥珠单抗组以及多西他赛+脂质体多柔吡星+贝伐单抗+曲妥珠单抗组。两个研究中,pCR均为主要或次要研究终点。
研究终点为新辅助曲妥珠单抗治疗后不同定义的pCR率,包括ypT0ypN0,ypT0/isypN0,ypT0/is。
结果
基本特征
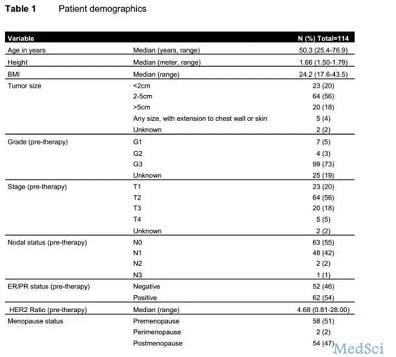
共纳入135名患者,其中65名及70名患者分别随机分配到ABCSG-24和ABCSG-32试验中,排除曲妥珠单抗为辅助治疗的32名患者,最终样本量为114。中位年龄50.3岁,中位BMI值24.2,大部分肿瘤为pT2(56%)且肿瘤分级为G3(73%)。HR+HER2+及HR-HER2+乳腺癌患者分别各占54.4%和45.6%。(表1)
HER2/CEP17与不同pCR定义间的关系
总体中位HER2/CEP17值为4.68。
ypT0ypN0:中位HER2/CEP17值分别为7.07(pCR)和4.58(非pCR);
ypT0/isypN0: HER2/CEP17值分别为7.00(pCR)和3.82(非pCR);
ypT0/is: HER2/CEP17值分别为7.07(pCR)和3.80(非pCR);
不同定义的pCR率:
ypT0/is 55.3%,ypT0/isypN0 53.3%,ypT0ypN0 45.3%;
图3为HER2/CEP17>6vs.≤6根据不同定义的pCR情况:
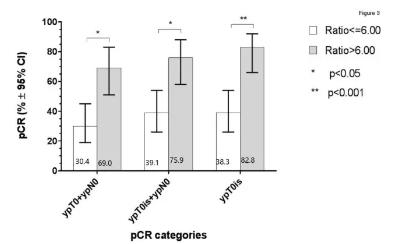
根据不同定义的pCR进行多因素分析均提示HER2/CEP17比值是pCR的唯一决定因素。
HR状态与pCR
本研究中HR状态与各种定义的pCR均无相关性。
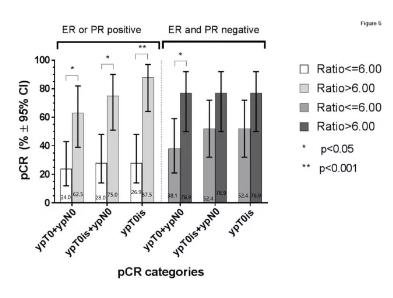
当pCR定义为ypT0/is或ypT0/isypN0时,在HR+HER2+乳腺癌患者中,HER2/CEP17>6者pCR均高于HER2/CEP17≤6者,这种相关性并未见于HR-HER2+乳腺癌患者中。当pCR定义为ypT0ypN0时,不论HR状态,HER2/CEP17>6者pCR均高于HER2/CEP17≤6者(图5)
讨论
本研究中选择HER2/CEP17=6作为阈值区分HER2扩增水平高低是基于我们的前期研究表明HER2+原发肿瘤中HER2/CEP17>6,对于未接受辅助曲妥珠单抗治疗的患者,提示首次出现转移更快。
NEOSPHERE和TRYPHAENA试验均是探讨新辅助抗HER2双靶治疗的疗效及安全性的。在NEOSPHERE研究中,帕妥株单抗使pCR从21.5%提升到39.3%。在TRYPHAENA研究中,三个试验组的ypT0N0及ypT0/is pCR率分别为51.9%,50.7%,45.3%和66.2%,61.6%,57.3%。本研究中,只使用了曲妥珠单抗单靶治疗,但总体pCR率均与上述两份研究的pCR率相当,我们认为这与曲妥珠单抗联合6周期化疗相关。
本研究不足:1.本研究中HER2并未统一检测;2.本研究中使用了两种不同ISH技术;3.样本量较小。
结论
本研究结果显示,不论新辅助治疗后是否残留DCIS成分,HER2/CEP17>6预示获得高pCR的可能性。未来可进一步探讨HER2/CEP17比值与新辅助抗HER2双靶治疗疗效的相关性。
点评:既往研究表明HER2+及三阴性乳腺癌患者在新辅助化疗后更容易获得病理完全缓解,高KI67值、年轻、肿瘤分级3级等均是与pCR相关的因素。而该研究中,尽管单因素分析中肿瘤分级G3是pCR的相关因素,但在多因素分析中却只有HER2/CEP17比值是pCR的预测因子。这从基因水平揭示了新辅助治疗对于高增值水平肿瘤的效果更佳。然而,针对HER2扩增水平的HER2/CEP17阈值目前暂无统一标准,需要更多、更大型的研究明确。另外,该研究中不同干预组间治疗方案有差异,不排除其他药物对pCR的影响。
原始出处:
Christian F. Singer, Yen Y. Tan, et al. Pathological Complete Response to Neoadjuvant Trastuzumab Is Dependent on HER2/CEP17 Ratio in HER2-Amplified Early Breast Cancer. Clinical Cancer Research.DOI: 10.1158/1078-0432.CCR-16-2373 Published July 2017
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#曲妥珠#
39
#新辅助#
27
好办法,希望能治理好。
69
#PCR#
34
谢谢分享,很不错。
52
学习了,涨知识
66