TAZVERIK(tazemetostat)治疗滤泡性淋巴瘤:FDA已批准其NDA
2020-02-15 Allan MedSci原创
Epizyme是一家开发表观遗传疗法的生物制药公司,今日宣布,美国食品药品监督管理局(FDA)已接受该公司的新药申请(NDA),以加速批准TAZVERIK™(tazemetostat)的上市。
Epizyme是一家开发表观遗传疗法的生物制药公司,今日宣布,美国食品药品监督管理局(FDA)已接受该公司的新药申请(NDA),以加速批准TAZVERIK™(tazemetostat)的上市。TAZVERIK(tazemetostat)用于治疗复发性或难治性滤泡性淋巴瘤(FL),这些患者至少接受过两次全身性治疗。
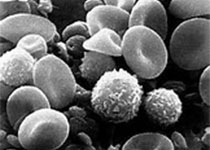
Epizyme首席医学官Shefali Agarwal博士说:“滤泡性淋巴瘤是一种无法治愈的疾病,患者需要一种安全、持久的治疗方法。如果获得批准,我们相信TAZVERIK能够为这些患者及其医生提供新选择”。滤泡性淋巴瘤在全世界占非霍奇金淋巴瘤(Non-Hodgkin lymphoma, NHL)的22%。滤泡性淋巴瘤最常见的表现是无痛性淋巴结肿大,典型表现为多部位淋巴组织侵犯,有时可触及滑车上淋巴结肿大。
原始出处:
https://www.firstwordpharma.com/node/1700908
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#AZ#
28
#MET#
34
#TAZVERIK#
33
#滤泡性淋巴瘤#
33
#NDA#
41
#Tazemetostat#
40