TAG:血小板与淋巴细胞百分比比指数是一种监测克罗恩病内镜活动度的简单非侵入性工具
2021-01-17 MedSci原创 MedSci原创
克罗恩病(CD)是一种慢性胃肠道炎症性疾病,其特征是复发和缓解反复交替。 大约一半的CD患者出现肠并发症,例如狭窄或瘘管。因此,在CD的整个疾病过程中,密切监
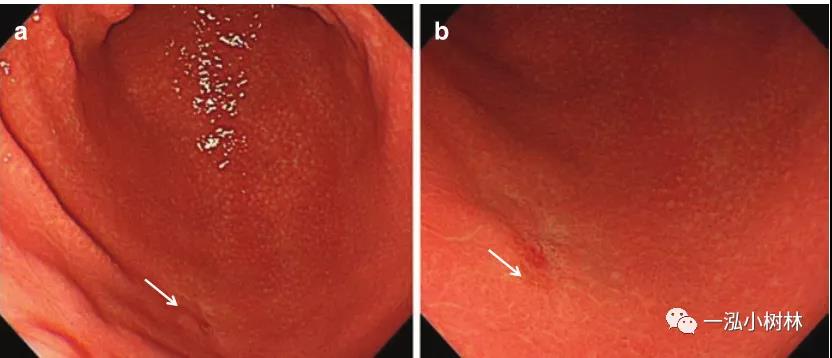
克罗恩病(CD)是一种慢性胃肠道炎症性疾病,其特征是复发和缓解反复交替。 大约一半的CD患者出现肠并发症,例如狭窄或瘘管。因此,在CD的整个疾病过程中,密切监视疾病活动至关重要。目前,内窥镜检查被认为是CD的疾病缓解程度的主要检查手段。然而,内窥镜检查是侵入性的,不舒适的,耗时且昂贵的,不适合常规开展。因此,需要精确和可靠的非侵入性的替代标志物,以评估CD内窥镜疾病活动的严重程度。最近的证据证明CD患者的全血细胞计数(CBC)异常。许多研究发现,一些常规的CBC血液指标,例如红细胞分布宽度,血小板计数,平均血小板体积和血小板生成比(PCT),都可以用作监测CD患者疾病活动的生物标志物。一些间接参数,例如嗜中性粒细胞与淋巴细胞之比和血小板与淋巴细胞之比,也已被用来确定疾病的活动度。因此,本项研究的目的是建立一个简单的模型,该模型由传统血液学检验的血液参数组成,可以可靠地反映CD内镜疾病活动的严重性。 研究人员对2016年至2020年间在中国四个三级医疗中心接受临床内镜检查的已确诊CD患者进行了回顾性分析。CD的简单内镜评分,CBC参数,C反应蛋白(CRP)水平,红细胞沉降的个体变量率和粪
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#非侵入性#
30
#侵入性#
43
很好的指标
63
#活动度#
35
挺好的指标可以用于科研
88
#内镜#
23
#淋巴细胞#
26
血小板淋巴细胞比 PLR
81
好文章,感谢分享。
100
好文章,共享之。
81