Pediatrics:新生儿紫绀型先天性心脏病的益生菌治疗结果
2021-09-23 从医路漫漫 MedSci原创
益生菌可以改变足月CCHD婴幼儿肠道内微生物群落结构和功能。动物研究和体外研究表明,益生菌的多种机制,如竞争性抑制病原体粘附受体结合位点,减少促炎细胞因子表达,增加抗炎细胞因子表达等

先天性心脏病(CHD)的发病率很高,占所有新生儿死亡的4%,患有冠心病的婴儿比健康婴儿更频繁地感染和使用抗生素。这些婴儿经常需要重大的外科手术、多次输血和延长住院时间,这可能会增加他们患败血症的风险。
在足月婴儿中,坏死性小肠结肠炎(NEC)很少见,常与先天性疾病有关。婴幼儿紫绀型CHD (CCHD)中NEC的发生率非常高。与心脏手术相关的炎症可能在这些婴儿NEC的发病机制中发挥作用
虽然婴幼儿冠心病NEC的确切发病机制尚不清楚,但急性肠系膜血流量减少和慢性紫绀都可能改变肠道菌群和肠道屏障的完整性,从而增加NEC的风险。有人提出,益生菌可以改变足月CCHD婴幼儿肠道内微生物群落结构和功能。动物研究和体外研究表明,益生菌的多种机制,如竞争性抑制病原体粘附受体结合位点,减少促炎细胞因子表达,增加抗炎细胞因子表达,分泌酶和有益的代谢产物,调节细胞氧化还原电位,增强上皮紧密连接的功能,诱导肠粘蛋白产生,与细胞表面分子的信号相互作用进行细胞保护和免疫反应(具有局部和全身效应),增加固有免疫抗菌肽的表达,以及引发神经内分泌和激素反应,这些反应与生长发育均有关。
据推测,预防性给予益生菌可能改变这一高危人群的肠道菌群改变,降低NEC风险。Ellis等人在最近的研究中指出,益生菌治疗可能有助于降低患有冠心病的婴儿NEC的发生率。然而,在美国国立卫生研究院国家医学图书馆(PubMed)的数据库或临床试验网站(ClinicalTrials.gov)的注册表中,都没有评估益生菌使用与婴幼儿冠心病发病率之间的关系的研究。因此,本研究旨在探讨口服益生菌对冠心病患儿预后的影响。
目的:研究口服益生菌对紫绀型先天性心脏病(CCHD)患儿预后的影响。
方法:采用前瞻性、盲法、随机对照试验评价合生药对冠心病患儿预后的影响。将冠心病患儿随机分为两组。研究组在母乳中加入合生素(乳酸双歧杆菌加菊粉)或混合喂养,直至出院或死亡。安慰剂组采用母乳喂养或混合喂养。结果测量为医院败血症、坏死性小肠结肠炎(NEC;BELL分期≥2),NICU住院时间和死亡。
结果:共纳入100例婴儿,每组50例。安慰剂组9例(18%),益生菌组2例(4%)(P= .03)。两组间NICU住院时间无差异(26 [14-36]vs32天[20-44],P=0.07]。安慰剂组有5例NEC(10%),益生菌组无NEC(P=0.03)。益生菌组死亡率较低,分别为5例(10%)和14例(28.0%),P=0.04)。
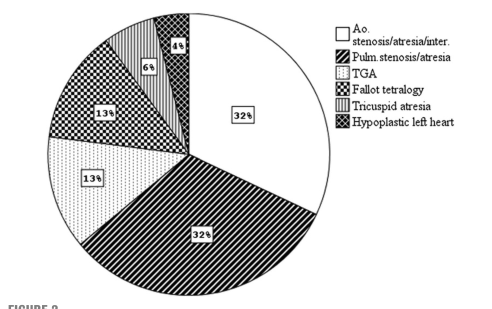
显示所有婴儿青紫型先天性心脏病类型的饼状图。Ao,主动脉;TGA,大动脉转位。
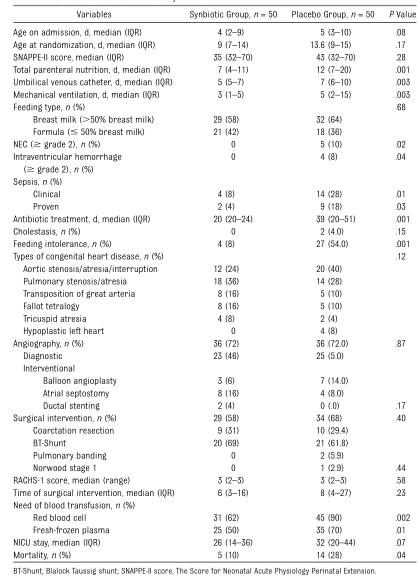
研究中婴儿的临床变量
结论:冠心病婴儿使用肠内益生菌可降低院内脓毒症、NEC和死亡的发生率。
原文出处
Dilli D, Aydin B, Zenciroğlu A,et al,Treatment outcomes of infants with cyanotic congenital heart disease treated with synbiotics.Pediatrics 2013 Oct;132(4)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
32
#DIA#
30
#Pediatric#
35
#先天性#
34
#治疗结果#
42
不错
65
不错
55
学习
51