J Clin Oncol:索拉非尼联合标准化疗治疗FLT3/ITD+急性髓系白血病患儿的疗效和安全性
2022-04-13 Nebula MedSci原创
在HAR FLT3/ITD阳性的急性髓系白血病患儿的常规化疗方案中加用索拉非尼是可行的,安全性好,并有望改善患儿的临床预后。
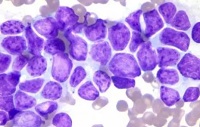
FLT3是一种受体酪氨酸激酶,约在10%-15%的新发急性髓系白血病(AML)儿童患者携带其突变。携带高等位基因比(HAR; AR>0.4)FLT3内部串联重复(ITD)突变的急性髓细胞白血病患儿预后较差,生存率约只有25%-30%;造血干细胞移植可将生存率提高至50%-65%。
COG AAML1031研究评估了在该患者人群的标准化疗方案中加用多激酶酪氨酸激酶抑制剂索拉非尼及采用索拉非尼单药维持治疗的效果和可行性。
受试患者被分成了三个队列。初始安全性探索阶段明确了诱导期索拉非尼的最大耐受剂量。队列2在诱导期加用索拉非尼治疗,队列3采用索拉非尼作单药维持治疗。在队列2/3的72位患者中进行了临床预后分析,并与只采用化疗未加用索拉非尼的76位 HAR FLT3/ITD+的AML患者进行了对比。
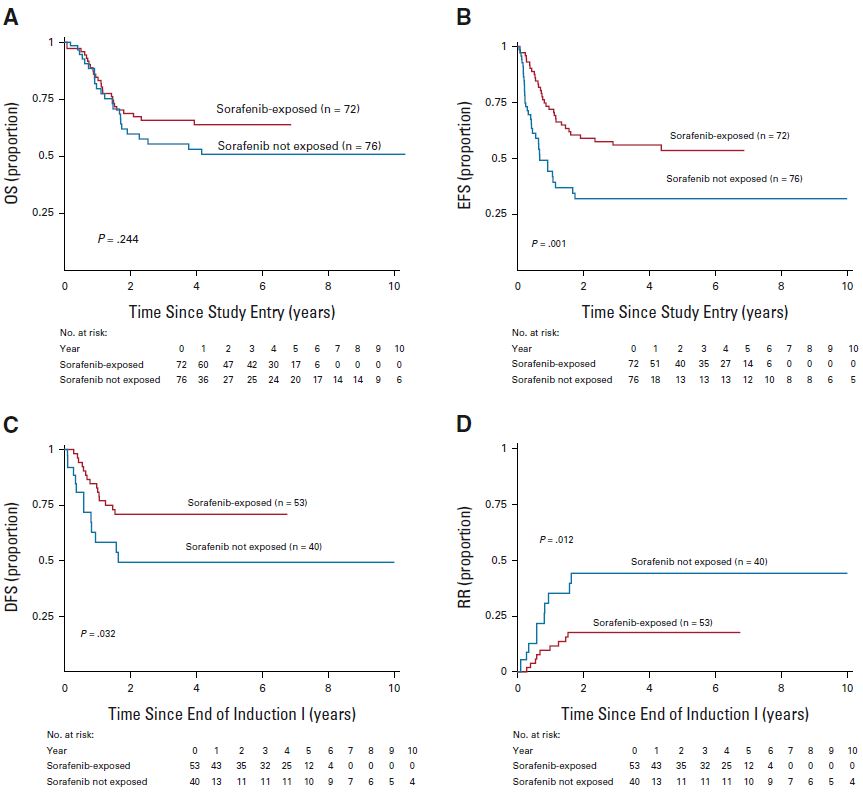
有无索拉非尼治疗的患者的总生存期(A)、无事件生存期(B)、无病生存期(C)和复发率(D)
索拉非尼的最大耐受剂量是200 mg/m2(1/日);剂量限制性包括红疹(n=2, 1例3级和1例2级)、2级手足综合征和3级发热。药代动力学/血浆抑制活性数据表明,测量的血浆浓度足以抑制磷酸化的FLT3。虽然在队列2和队列3中,索拉非尼的疗效显著,但接受索拉非尼治疗的患者也相比对照人群更可能进行造血干细胞移植。
索拉非尼的药代动力学/药效学效应
对造血干细胞移植和有利的共发生突变的多变量分析证实了索拉非尼的益处。具体而言,未采用索拉非尼治疗的HAR FLT3/ITD+患者发生某些终点事件的风险大约是接受索拉非尼治疗的患者的两倍(无事件生存的风险比[HR] 2.37, p<0.001;完全缓解后无病生存的HR 2.28,p=0.032;完全缓解后的复发风险 HR 3.03, p=0.010)。
综上,该研究显示,在HAR FLT3/ITD阳性的急性髓系白血病患儿的常规化疗方案中加用索拉非尼是可行的,安全性好,并有望改善患儿的临床预后。
原始出处:
Jessica A. Pollard, et al. Sorafenib in Combination With Standard Chemotherapy for Children With High Allelic Ratio FLT3/ITD+ Acute Myeloid Leukemia: A Report From the Children's Oncology Group Protocol AAML1031. Journal of Clinical Oncology. March 29, 2022. https://ascopubs.org/doi/full/10.1200/JCO.21.01612
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
39
#疗效和安全性#
39
#标准化#
31
#标准化疗#
39
#髓系白血病#
32
#FLT3#
30