Radiology:IVIM序列在新诊断AML中的预后价值
2021-05-07 shaosai MedSci原创
急性髓系白血病(AML)是一种预后极差的血液系统疾病,只有40%的年轻人和10%的老年人具有长期生存率。

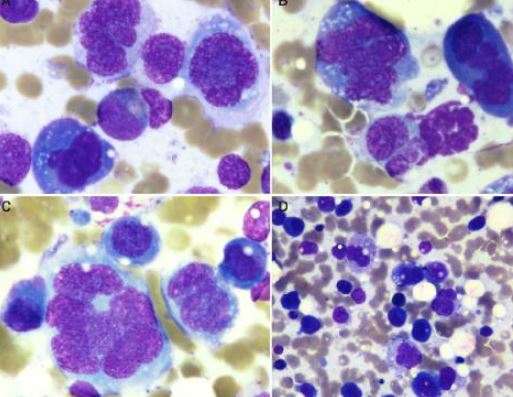
急性髓系白血病(AML)是一种预后极差的血液系统疾病,只有40%的年轻人和10%的老年人具有长期生存率。在AML的进展过程中,白血病细胞可浸润正常骨髓,导致肿瘤细胞的增殖和肿瘤血管生成。一些研究证实,细胞增殖和血管生成的增加是AML的预后因素。
可通过有创髂骨活检来量化血管生成和骨髓细胞数量,但该方案可由于取样偏差导致结果错误。体素内不相干运动(IVIM)MR成像是扩散加权成像方法的一种,该技术使用多个b值和双指数信号模型,能够产生反映组织微血管灌注和组织扩散率的定量参数。在低b值(例如,200秒/mm2)时,伪灌注分数f和伪扩散系数D*可以评价灌注特性;在高b值(如200到1000秒/mm2)时,扩散系数D可以反映与组织细胞密度有关的水的扩散。虽然IVIM参数的病理生理学意义有待进一步研究(15),但多项研究表明,f和D值是评估实体和血液肿瘤中血管生成的血管体积分数和细胞数量的影像学标志物。
近日,发表在Radiology杂志的一项研究探讨了骨髓IVIM参数是否能预测新诊断AML患者的总生存期(OS),为临床早期、准确且无创的评估AML患者的预后提供有价值的参考依据。
本项前瞻性研究连续招募了2014年7月至2016年3月间的新诊断AML患者。每位患者均接受了包括IVIM序列的腰椎MRI检查。收集参与者的临床特征和OS。中位随访时间为20个月(范围1-56个月)。IVIM参数(伪灌流分数f;扩散系数D;伪扩散系数D*)。使用非参数log-rank检验来确定预测OS的IVIM参数阈值。采用单变量Kaplan-Meier和多变量Cox比例风险回归分析来评估指标的预后意义。
本研究共对53名患者(平均年龄42±17岁;30名男性)进行了评估。非参数log-rank检验结果显示,OS的f值阈值为31.0%,D值为0.2 × 10-3 mm2/sec。单因素分析表明,高f值(>31.0%)和低D值(≤0.2 × 10-3 mm2/sec)与较短的OS相关(P分别为0.003和0.01)。f值大于31.0%(风险比,2.4;95%置信区间:1.0,5.6;P = 0.046)与OS相关,在多变量分析中不受临床混杂因素(年龄、核型和白细胞计数)的影响。
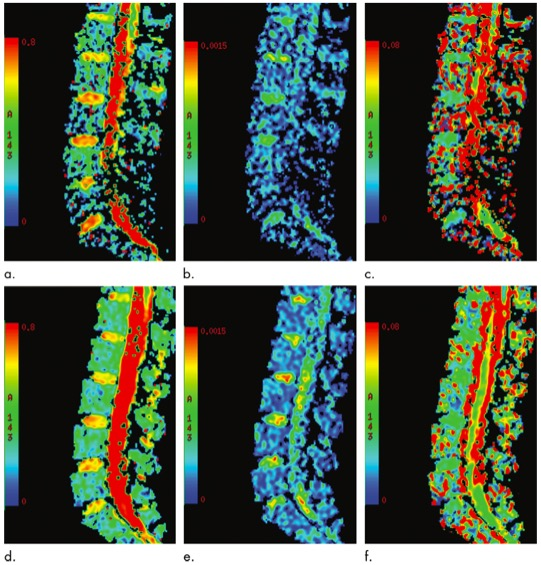
图 两位患者的f(a, d) 、D(b, e) 和D *(c, f) 系数的IVIM MRI参数图。(a-c)总体生存期为40个月的25岁男性患者的IVIM MRI参数图。该图显示了(a)一个较低的 f值(25.7%),(b) 较高的D值(0.26× 10-3 mm2/sec), (c) 较低的D*值(81× 10-3 mm2/sec)。(d-f)总体生存期为3个月的22岁女性患者的IVIM MRI参数图。该图显示了(d)一个较高的f值 (33.6%),(e)较低的d (0.19 × 10-3 mm2/sec), (f)较低的d * (101× 10-3 mm2/sec)。
本研究表明,IVIM MRI参数f值较高及D值较低预示急性髓系白血病(AML)患者预后不良,同时f值是一个独立的总生存率预测因子。综上所述,IVIM MRI参数可协助临床用于制定AML患者的个体化治疗方案,为提高AML患者预后提供了影像学支持。
原文出处:
Jianting Li,Wenjin Li,Jinliang Niu,et al.Intravoxel Incoherent Motion Diffusion-weighted MRI of Infiltrated Marrow for Predicting Overall Survival in Newly Diagnosed Acute Myeloid Leukemia.DOI:10.1148/radiol.2020191693
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#IVIM#
44
看看原文 不错
54
#新诊断#
31
#预后价值#
49
学习
65