中心点:与一般人群相比,血友病患者颅内出血的发生率和死亡率均明显更高。
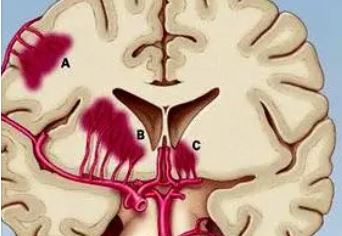
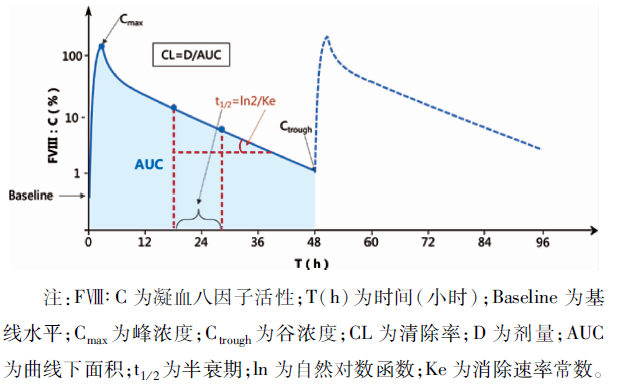
A型血友病和B型血友病是一种以X染色体-连锁的方式遗传的凝血因子VIII(FVIII)或IX(FIX)缺乏为特征的出血性疾病。颅内出血 (ICH) 是血友病患者中较为常见的一种严重并发症。
近期,国际一流期刊《血液》上发表了一篇Meta分析“Incidence and mortality rates of intracranial hemorrhage in hemophilia: a systematic review and meta-analysis”,汇总分析了颅内出血在血友病患者中的发生率和致死率。
研究人员采用与“血友病”、“颅内出血”或“死亡率”相关的词条系统地检索了PubMed和EMBASE数据库,纳入了评估血友病患者颅内出血发生率或死亡率且患者人数≥50的研究,在三个年龄组(所有年龄段的血友病患者、儿童和25岁以下年轻患者、新生儿血友病患者)中分别汇总计算了血友病患者颅内出血的发生率和死亡率。
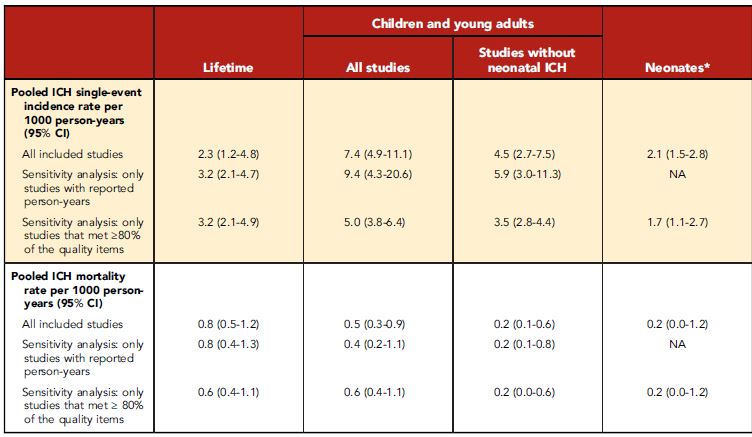
血友病患者颅内出血的发生率和死亡率的汇总数据
筛选到45项符合要求的研究,共涵盖54470位患者,共随访了809151人·年,包括5326名新生儿。在所有年龄段患者人群中,颅内出血的发生率和死亡率分别是2.3(95% CI 1.2-4.8)和0.8(0.5-1.2)/1000人·年。在儿童和年轻患者中,颅内出血的发生率和死亡率分别是7.4 (95% CI 4.9-11.1)和0.5 (95% CI 0.3-0.9)/1000人·年。在确诊血友病的新生儿中,颅内出血的累积发生率是2.1%(95% CI 1.5-2.8)/100次活产。35%-58%的颅内出血都是自发性的。
综上,该研究结果证实,颅内出血可发生在任何年龄的血友病患者,严重威胁血友病患者的生命安全,需要采取适当的预防措施。
原始出处:
Anne-Fleur Zwagemaker, et al. Incidence and mortality rates of intracranial hemorrhage in hemophilia: a systematic review and meta-analysis. Blood. December 30, 2021. https://doi.org/10.1182/blood.2021011849.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发生率#
47
#致死率#
40
已学习,新知识
67
学习一下
72
学习了
78