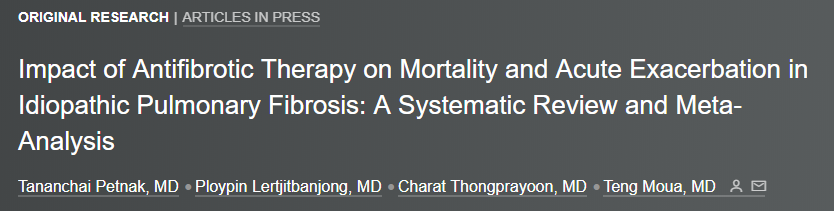
Chest:抗纤维化治疗对特发性肺纤维化患者死亡率和急性加重的影响
2021-07-08 MedSci原创 MedSci原创
抗纤维化治疗似乎降低了IPF患者的全因死亡率和AE风险。
特发性肺纤维化(IPF)是一种进行性纤维化间质性肺疾病,与显著的发病率和死亡率相关。尼达尼布和吡非尼酮是目前批准用于减缓IPF肺功能下降速度的两种抗纤维化药物,但有关治疗对死亡率和急性加重(AE)风险影响的信息仍然有限或未知。

近日,呼吸领域权威杂志chest上发表了一篇研究文章,该研究旨在明确抗纤维化治疗是否会降低死亡率和AE风险。
研究人员对多个数据库进行了全面检索,包括Ovid MEDLINE(R)、Ovid Embase、Ovid Cochrane Central Register of Controlled Trials、Ovid Cochrane Database of Systematic Reviews和Scopus。如果研究比较了接受和未接受抗纤维化治疗的IPF患者死亡率或AE事件,则纳入分析。研究人员使用随机效应荟萃分析和逆方差法汇总了伴有95%置信区间(CI)的相对风险(RR),并评估了全因死亡率和急性加重(AE)风险这两个主要结局。
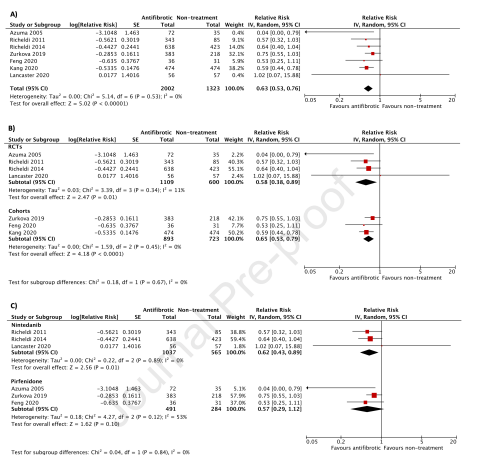
该荟萃分析总共纳入了26项研究(8项随机对照试验和18项队列研究),共计12956名患者。抗纤维化治疗与全因死亡风险降低相关,汇总RR为0.55(95%CI为0.45-0.66),I2为82%。这种效应在其他亚组分析中是一致的,包括按研究类型、偏倚风险、随访持续时间和抗纤维化亚型进行分层。抗纤维化治疗还降低了AE的风险,合并RR为0.63(95%CI为0.53-0.76),I2为0%。对于尼达尼布,研究类型和亚组分析对AE风险的影响是一致的,对于吡非尼酮则不同。
由此可见,抗纤维化治疗似乎降低了IPF患者的全因死亡率和AE风险。
原始出处:
Tananchai Petnak.et al.Impact of Antifibrotic Therapy on Mortality and Acute Exacerbation in Idiopathic Pulmonary Fibrosis: A Systematic Review and Meta-Analysis.chest.2021.https://doi.org/10.1016/j.chest.2021.01.081
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#特发性#
34
#抗纤维化#
43
#患者死亡#
33
#EST#
33
#Chest#
48
#急性加重#
45
6默默看看
56