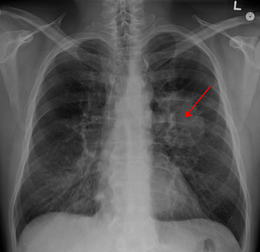
J Clin Oncol:年龄对非小细胞肺癌死亡率有何影响?
2017-04-13 选题审校:韩茹 编辑:吴星 环球医学编译
专家点评:几日前,一篇癌症与运气的文章的发表给大家同样带来不少的震动。癌症,作为医学界一直致力于攻克的难题,结题点到底在哪里。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非小细胞#
40
#Oncol#
26
#肺癌死亡率#
40
mark
59
mark
62
很好,学习了很好很多知识。
63