Diabetes Care:不论胖瘦、有无微血管疾病,杜拉鲁肽都能降低HbA1c
2022-03-11 MedSci原创 MedSci原创
杜拉鲁肽1.5毫克的治疗与72个月内HbA1c的长期下降有统计学关系,且该作用与基线糖尿病持续时间、微血管疾病和BMI无关。
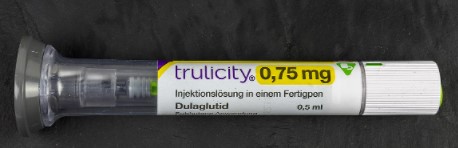
降糖可以减少高血糖的症状和许多糖尿病的长期并发症。患者的特点可能会影响对各种疗法的血糖反应。胰高血糖素样肽-1(GLP-1)受体激动剂是一类用于治疗2型糖尿病的降糖药,包括杜拉鲁肽。AWARD试验表明,杜拉鲁肽6个月的降糖效果与BMI和糖尿病持续时间无关。这些特征或微血管疾病的存在是否会影响短期或长期治疗期间的降糖效果仍是未知数。
REWIND 心血管(CV)结果试验表明,在2型糖尿病和CV风险因素或以前的CV疾病(CVD)的标准护理中加入杜拉鲁肽1.5毫克,可降低2型糖尿病患者CV死亡、非致命性心肌梗死或非致命性中风等综合结果的危险。
为了在 REWIND试验的事后分析中,评估杜拉鲁肽1.5mg治疗患者的参与者特征和糖化血红蛋白(HbA1c)水平的长期变化,来自加拿大麦克马斯特大学和汉密尔顿健康科学研究所的专家开展了相关研究,结果发表在Diabetes Care杂志上。

在调整糖尿病病程、先前的微血管疾病(肾病或视网膜病变)和BMI之前和之后,研究人员评估了治疗期间和最长72个月的HbA1c从基线的变化。斜率分析用于评估治疗0-12个月和12-72个月期间HbA1c的变化。
结果显示,与安慰剂相比,在72个月的治疗期间,接受杜拉鲁肽治疗的患者的HbA1c明显降低(最小二乘平均差=-0.61%,P<0.001),且该作用与糖尿病病程、既往微血管疾病和BMI无关(所有交互作用P>0.07)。所有时间点都有明显的减少,并且与这些基线特征无关。
斜率分析显示,与安慰剂组相比,杜拉鲁肽组在调整前和调整后0-12个月的HbA1c降低率较高。与安慰剂组相比,杜拉鲁肽组从12个月到72个月的HbA1c增加率也较高,在调整了糖尿病持续时间、先前的微血管疾病和BMI组合后变得不明显。尽管在此期间杜拉鲁肽组的HbA1c增加率较高,但杜拉鲁肽组的平均HbA1c值仍低于基线,低于安慰剂组的平均HbA1c值。

由此可见,杜拉鲁肽1.5毫克的治疗与72个月内HbA1c的长期下降有统计学关系,且该作用与基线糖尿病持续时间、微血管疾病和BMI无关。
参考文献:
HbA1c Reduction in Dulaglutide-Treated Patients Irrespective of Duration of Diabetes, Microvascular Disease, and BMI: A Post Hoc Analysis From the REWIND Trial. Diabetes Care 1 March 2022; 45 (3): 547–554. https://doi.org/10.2337/dc21-1160
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#DIA#
40
#杜拉鲁肽#
47
学习了
62
#HbA#
51
#Diabetes#
48
#BET#
37
学习~
56
#微血管#
33
#血管疾病#
39
#微血管疾病#
35