Clin Gastroenterology H:肿瘤坏死因子拮抗剂在原发性硬化性胆管炎患者中的作用分析
2020-08-30 MedSci原创 MedSci原创
原发性硬化性胆管炎(PSC)是一种特发性且异质性很大的肝胆疾病,主要特点是进展性的胆管炎症及纤维化,最终造成胆汁郁积。
原发性硬化性胆管炎(PSC)是一种特发性且异质性很大的肝胆疾病,主要特点是进展性的胆管炎症及纤维化,最终造成胆汁郁积。原发性硬化性胆管炎的发病机理尚不清楚,目前临床上也缺乏有效的治疗手段,小部分的患者可以通过肝移植存活。而PSC合并炎症性肠病(IBD)的患者更是少见,IBD患者经常使用抗肿瘤坏死因子进行治疗,那么抗肿瘤坏死因子在PSC中的作用还没有研究进行报道,本项研究旨在进行相关研究。

研究人员对接受抗肿瘤坏死因子(TNF)(英夫利昔单抗或阿达木单抗)治疗的141例PSC和IBD患者进行了回顾性分析。收集测定了他们的血清碱性磷酸酶(ALP)水平。IBD获得反应定义为内镜反应或者临床反应。最后使用线性回归分析来确定与抗TNF治疗期间ALP水平显着相关的因素。研究结果显示抗TNF治疗在48%的IBD患者中获得缓解反应。药物暴露前后PSC症状发生率无差异。停用抗TNF的最常见原因是IBD的原发性无反应(17%)和副作用(18%)。在3个月时,用英夫利昔单抗治疗的患者血清ALP中位数降低了4%,相比之下,接受阿达木单抗治疗的患者中ALP降低了15%( P= .035)。与较低ALP相关的因素是基线时的正常ALP(P <.01)。
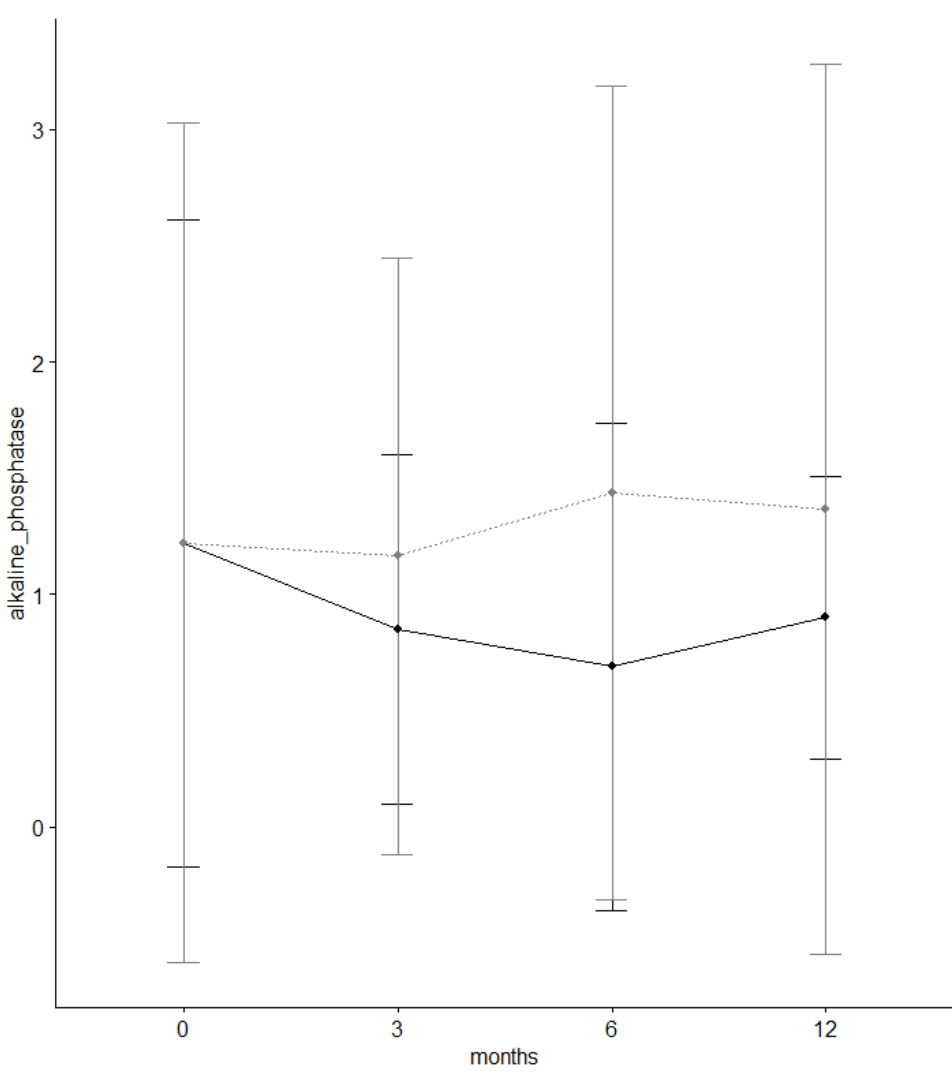
(阿达木单抗效果更好)
本项研究对141例PSC和IBD患者进行的回顾性分析后发现,抗TNF药物疗效中等,并且与PSC症状加重或特定副作用无关。但是阿达木单抗的使用与血清ALP降低是凉后预后的预测因素。
原始出处:
Charlotte Rose Hawkey Hedin. Et al. Effects of Tumor Necrosis Factor Antagonists in Patients With Primary Sclerosing Cholangitis. Clin Gastroenterology H.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#GAS#
34
#Gastroenterol#
31
#原发性#
40
#AST#
32
#坏死#
38
#原发性硬化性胆管炎#
60
#肿瘤坏死因子#
33
#硬化性#
35
#Gastroenterology#
35
#拮抗剂#
37