Am J Respir Cell Mol Biol:他汀类药物是特发性肺纤维化的调节剂
2020-05-25 MedSci原创 MedSci原创
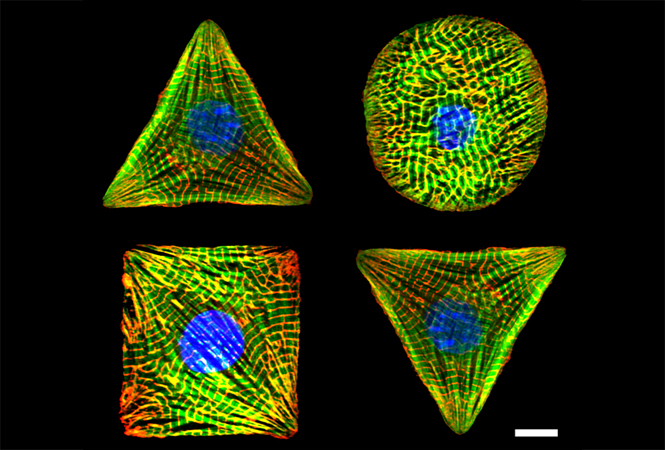
特发性肺纤维化是一种治疗方案有限的肺部疾病,其特点是病理性的成纤维细胞活化和瘢痕形成的肺部重塑异常。YAP(是相关蛋白)是一种转录共激活因子,可介导控制成纤维细胞激活的机械和生化信号。在这项研究中,我
特发性肺纤维化是一种治疗方案有限的肺部疾病,其特点是病理性的成纤维细胞活化和瘢痕形成的肺部重塑异常。YAP(是相关蛋白)是一种转录共激活因子,可介导控制成纤维细胞激活的机械和生化信号。在这项研究中,我们开发了一种高通量小分子筛选剂,用于筛选原代人肺成纤维细胞中的YAP抑制剂。
结果发现,多种HMG-CoA(羟甲基戊二酰辅酶A)还原酶抑制剂(他汀类药物)通过诱导YAP磷酸化,胞质保留和降解来抑制YAP核定位。进一步研究表明,甲羟戊酸途径调节YAP激活,辛伐他汀治疗可减少激活的人肺成纤维细胞和博来霉素小鼠肺纤维化模型中的纤维化标记。最后,我们发现辛伐他汀在小鼠肺成纤维细胞体内调节YAP。
总之,我们的结果突出了小分子筛选YAP抑制剂的潜力,并为他汀类药物在特发性肺纤维化中的抗纤维化活性提供了机制。
原始出处:
Daniela M Santos, Lorena Pantano, et al., Screening for YAP Inhibitors Identifies Statins as Modulators of Fibrosis. Am J Respir Cell Mol Biol. 2020 Apr;62(4):479-492. doi: 10.1165/rcmb.2019-0296OC.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
48
#特发性#
33
#Bio#
40
#Cell#
38
#Biol#
57
#他汀类药#
37
他汀类药物越来越有价值了
115