Blood:特发性多中心Castleman病的mTOR激活增强
2020-04-01 MedSci原创 MedSci原创
在特发性多中心Castleman病(iMCD)中,mTOR通路被过度激活,并被作为候选新型治疗靶点。 mTOR在iMCD中的激活程度与mTOR驱动的自身免疫性淋巴组织增生综合征的相似。
特发性多中心Castleman病(iMCD)是一种罕见且难以理解的血液病,其特征为淋巴结病、全身性炎症、血细胞减少和威及生命的多器官功能障碍。白介素6(IL-6)抑制可有效治疗约1/3的患者。由于病因、失调细胞类型和信号传导通路尚不明确,导致对IL-6无反应者的选择有限。
Arenas等人曾报道过三例mTOR活化增强的抗IL-6的无反应者,他们对西罗莫司抑制mTOR有应答。在本研究中,Arenas等人对来自iMCD患者和对照的组织和血清蛋白质组中的mTOR信号进行研究。
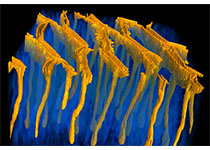
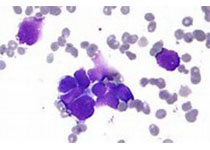
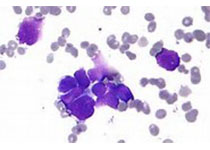
通过免疫组化(IHC)检测了iMCD患者(26例)和健康对照的淋巴结中的pS6、p4EBP1和p70S6K(众所周知的mTORC1激活的效应分子和指标),结果显示与健康对照相比,iMCD患者淋巴结的小泡间间隙中mTOR激活增加。此外,IHC检测pS6还显示,iMCD的mTOR激活程度还高于霍奇金淋巴瘤、系统性红斑狼疮和反应性淋巴结的,提示iMCD中的mTOR激活不仅是淋巴增生/炎性淋巴结病的产物。
此外,iMCD中mTOR的激活程度可与自身免疫性淋巴组织增生综合症的相媲美,后者是由mTOR过度活化所引起的对西罗莫司治疗有反应的一种疾病。
对iMCD患者(88例)和对照(42例)的血清蛋白质组数据的基因集富集分析显示,mTORC1信号明显富集。最后,功能性研究显示,与健康对照相比,iMCD缓解期患者的样本中外周单核细胞和T细胞的基线mTOR通路活化增加。
IL-6刺激可增强iMCD患者的mTOR激活,JAK1/2抑制可抵消这一效应。
综上所述,本研究表明mTOR激活可作为iMCD患者的新治疗靶点(现已通过西罗莫司的试验进行研究)。
原始出处:
Daniel J Arenas, et al. Increased mTOR activation in idiopathic multicentric Castleman disease. Blood. March 23, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#特发性#
30
#AST#
32
#多中心#
29
#EMA#
37
#Castleman病#
39
#Cas#
30