JACC:超薄冠脉药物洗脱支架植入远期预后更佳
2018-12-25 MedSci MedSci原创
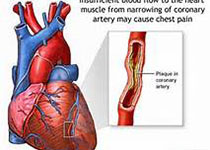
冠脉药物洗脱支架的发展以及引进了新的金属合金材料,改变了支架的金属构造和生物可吸收聚合物,但这些改进带来的安全性和有效性在之前的研究中结果是不一致的。本研究的目的旨在比较和评估超薄支柱(60μm)生物可吸收聚合物西罗莫司洗脱支架(BP SES)和薄支柱(81μm)耐用聚合物伊维莫司洗脱支架(DP EES)的远期安全性和有效性。本次临床研究为BIOFLOW V临床试验,旨在比较BP SES和DP E
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
25
#远期预后#
41
#支架植入#
42
#洗脱支架#
37
#药物洗脱支架#
39
#ACC#
24
#植入#
31
敲黑板画重点
80