J Thorac Oncol:miR-17下调LKB1提示预后较差的NSCLC患者可采用能量应激治疗
2021-05-02 Nebula MedSci原创
高表达miR-17的野生型LKB1 NSCLC可能对能量应激条件敏感,或有资格接受基于代谢脆弱的治疗干预
近期,临床前模型揭示了LKB1/KRAS共突变的非小细胞肺癌(NSCLC)对代谢应激治疗的易感性。由于miR-17是LKB1潜在表观遗传调控因子,Cristina等人推测,高表达miR-17的野生型LKB1 NSCLC可能对能量应激条件敏感,或有资格接受基于代谢脆弱的治疗干预。
研究人员采用了KRAS突变和LKB1缺失的不同组合的NSCLC细胞株,以及miR-17高表达(L/miR17H)或低表达(L/miR17L)的患者来源的异种移植(PDX),评估了LKB1通路损伤和对二甲双胍的凋亡反应。此外,研究人员还回顾性评估了LKB1和miR-17在NSCLC患者和PDXs组织标本中的表达水平。最后,还采用TCGA数据集的一个肺癌队列分析了miR-17的表达及其与临床特征的潜在相关性。
分析结果显示,miR-17是NSCLC中LKB1的表观遗传调控因子。荧光素酶报告实验证实,miR-17靶向于LKB1 3'非编码区。miR-17过表达在功能上影响了LKB1/AMPK通路。
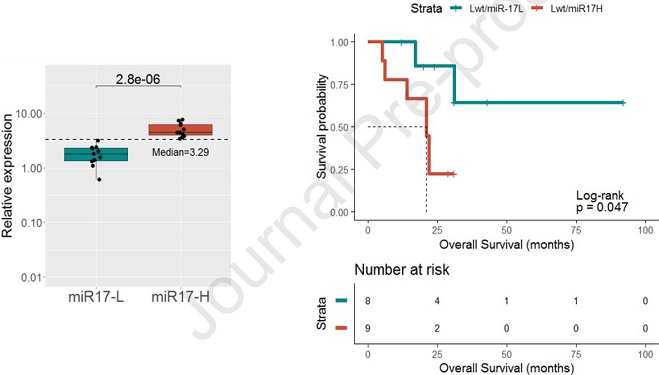
miR-17在PDX中的表达水平与肿瘤来源患者的OS的相关性
二甲双胍处理仅在LKB1WT细胞株和LWT/miR17H PDX细胞中可诱导miR-17过表达后诱导细胞凋亡。对NSCLC患者的回顾性分析显示,miR-17与LKB1的表达呈负相关,并强调了miR-17在LKB1WT患者中的预后作用,TCGA数据分析进一步证实了这一点。
总而言之,该研究发现miR-17是LKB1在NSCLC肿瘤中表达的中介因子。这项研究提出了一个miR-17表达评分,或可用来区分LKB1表达受损和预后不良的LKB1WT NSCLC患者,这些患者或可接受基于能量应激的治疗。
原始出处:
Borzi Cristina,Ganzinelli Monica,Caiola Elisa et al. LKB1 down-modulation by miR-17 identifies NSCLC patients with worse prognosis eligible for energy-stress based treatments. J Thorac Oncol, 2021, https://doi.org/10.1016/j.jtho.2021.04.005
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#SCLC患者#
31
#Oncol#
22
#miR#
30
#THORAC#
26
#NSCLC患者#
35
#应激#
26
#LKB1#
34
JTO上有很多不错的好文章,谢谢梅斯及时上新
49
谢谢梅斯分享这么多精彩信息
51
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
53