JAMA:肌内神经束内 TDP-43 积聚可能是肌萎缩侧索硬化患者的一种新型诊断生物标志物。
2022-05-28 影像小生 MedSci原创
轴突 pTDP-43 积累可能是 ALS 患者的特征
肌萎缩性侧索硬化症(ALS)患者的肌肉组织中是否存在特殊的病理标志物?在10例尸检患者的双病例对照研究和114例连续患者的队列研究中,散发性ALS (SALS)患者肌内神经束中存在磷酸化的交互反应DNA结合蛋白43 (pTDP-43)阳性轴突。114例无ALS家族史或其他神经肌肉疾病的患者行肌肉活检,所有轴突pTDP-43阳性神经束的患者活检后均诊断为SALS。本研究结果提示肌内神经束轴突积聚可能是ALS患者的特征。
神经肌肉接头和轴突的退化被认为是肌萎缩侧索硬化症 (ALS) 发病机制的一个重要方面。然而,反式反应 DNA 结合蛋白 43 (TDP-43) 在轴突中的作用的机制尚未在病理学上得到阐明。
Takashi Kurashige等在JAMA期刊发表研究文章,目的是识别和表征ALS患者骨骼肌外周轴突的组织病理学特征。
该研究包括 2 个部分:尸检病例对照研究和至少 1 年随访的回顾性基于人群的队列研究。队列研究的患者于 2004 年 1 月 1 日至 2019 年 9 月 30 日入组。尸检研究包括患有 TDP-43 病理学的散发性 ALS (SALS) 患者和患有非 ALS 疾病的对照患者。该队列研究招募了没有 ALS 或其他神经肌肉疾病家族史的患者,以及活检未诊断出患有肌肉疾病的患者。数据于 2019 年 9 月至 2021 年 6 月期间收集,并于 2021 年 6 月进行分析。进行肌肉活检或死后肌肉组织检查。
该研究中
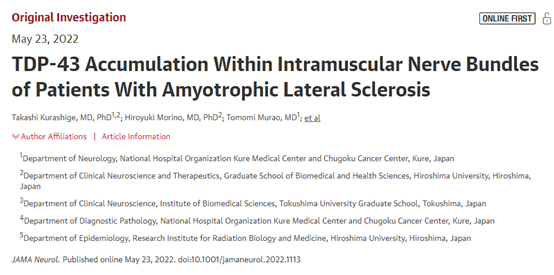
1. 共有 10 名尸检证实的 SALS 患者(死亡时的平均 [SD] 年龄,76.1 [8.5] 岁;
1.1. 8名男性[80%])表现为肌内神经束轴突磷酸化TDP-43 (pTDP-43)阳性积累。
1.2. 无ALS 的 12 名对照患者没有。
尸检病例对照研究中骨骼肌肌内神经束中轴突pTDP-43阳性积累
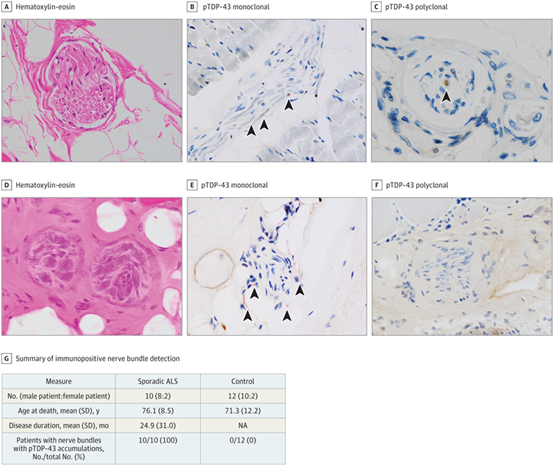
2. 在队列研究的 114 名患者中(平均 [SD] 年龄,62.3 [16.1] 岁;76 名男性 [67%]),71 名患者(62.3%)表现出肌内神经束;43 例(37.7%) 没有。
2.1. 在表现出 pTDP-43 阳性肌内神经束的患者中,33 名患者(22 名男性 [66.7%];平均 [SD] 年龄,65.2 [15.6] 岁)后来被诊断为 ALS。
2.2. 其他 38 名患者(26 名男性 [68.4%];平均 [SD] 年龄,59.3 [18.0] 岁)没有显示 pTDP-43 阳性束,也没有发展为 ALS。
2.3. 在那些没有明显神经束的人中(28 名男性 [65.1%];平均 [SD] 年龄,61.3 [15.3] 岁),3 人后来被诊断出患有 ALS。
2.4. 在活检队列中的 ALS 患者中,9 名 pTDP-43 阳性束在活检时仅表现出较低的运动神经元症状。
在肌活检队列中,最终发展为肌萎缩侧索硬化症(ALS)的患者肌内神经束中出现轴突pTDP-43阳性积累
这项双重病例对照和回顾性队列研究的结果表明轴突 pTDP-43 积累可能是 ALS 患者的特征。神经束中的 TDP-43 可能是 ALS 的一种新型诊断生物标志物。
原文出处
TDP-43 Accumulation Within Intramuscular Nerve Bundles of Patients With Amyotrophic Lateral Sclerosis. JAMA Neurol. Published online May 23, 2022. doi:10.1001/jamaneurol.2022.1113
https://jamanetwork.com/journals/jamaneurology/fullarticle/2792745
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#萎缩#
49
#标志物#
52
#TDP-43#
69
#肌萎缩#
47
#肌萎缩侧索硬化#
52
#生物标志#
22
#生物标志#
32
JAMA上文章都是顶级的,谢谢梅斯及时上新
27
不错,学习了。
0