Neurology:功能MRI:ALS伴认知和行为损害或为ALS的表型变异
2021-12-05 Naomi MedSci原创
近日,研究人员使用MRI连接数据的模型破译ALS-FTD频谱中共有及独立的神经关联。ALS-CBI的功能重排具有适应不良的作用,并伴有与ALS-CN相似的结构改变,ALS-CBI可能是表型变异。
肌萎缩侧索硬化症(ALS)是运动神经元病最常见的临床表现,其特征是上下运动神经元进行性变性。越来越多的证据支持肌萎缩侧索硬化症和广泛的额颞叶痴呆(FTD)之间的临床、病理和遗传重叠的概念。事实上,至少50%的ALS患者在病程中出现认知症状(主要影响执行功能)和行为改变,导致5-25%的病例被全面诊断为FTD。考虑到ALS患者并发认知障碍是一个已知的负面预后因素,与更快的死亡或气管切开术相关,对这种情况有更好的定义和理解具有明显的临床意义。
修订后的Strong标准为ALS-FTD临床连续体建立了一个公认的命名,范围从ALS认知正常(ALS-CN)到ALS伴FTD(ALS-FTD),包括ALS伴认知损害(ALS-CI)、ALS伴行为损害(ALS-BI)和ALS伴认知和行为损害(ALS-CBI)。然而,目前对于ALS-CN与ALS-CI/BI和ALS-FTD病例的病理基础,以及这是否被认为是ALS的一种不同的表型或ALS的自然演变仍存在着很大的争议。横断面研究报告了ALS-ci/bi在有更严重运动障碍的疾病阶段的比例增加,甚至已经提出了ALS的序贯认知分期系统,反映了TDP-43沉积的病理阶段。然而,少数可用的ALS纵向神经心理学研究的结果存在分歧,因为一些支持认知和行为变化的稳定性,而另一些则表明认知障碍的微妙进展。
在此背景下,先进的磁共振成像(MRI)为研究ALS和FTD的脑结构提供了有用的工具。几项MRI研究使用传统的MRI和连接方法评估了FTD的行为变异型(BV-FTD)患者,报告了额岛和颞叶网络内结构和功能损害的特定模式。在ALS患者中,与ALS-CN患者相比,认知障碍患者广泛存在灰质(GM)和白质(WM)损害,不仅涉及运动,而且还涉及运动外区域,包括额颞区、顶区、岛区和扣带区。最近一项使用连接方法的研究显示,与ALS-CN患者相比,ALS-CBI患者广泛的大脑WM改变影响额颞区。现有的功能MRI研究报告了相互矛盾的结果,因为ALS的执行功能障碍和行为障碍与额顶和颞叶网络的功能连通性增强或额顶、突起和执行网络的连通性受到抑制有关。然而,在目前的文献中,缺乏专门评估ALS-CBI患者额颞区功能改变的MRI研究。
到目前为止,ALS-CBI与ALS-FTD频谱的相反两端(即ALS-CN和成熟的FTD)的脑网络重组的直接评估仍然是必要的。此外,还没有研究利用图表分析和连接学将结构和功能信息结合起来,来调查不同谱系患者认知和行为下降的神经相关性。近日,有研究人员使用MRI连接数据的数学模型来破译ALS-FTD频谱中共同的和不同的神经关联。
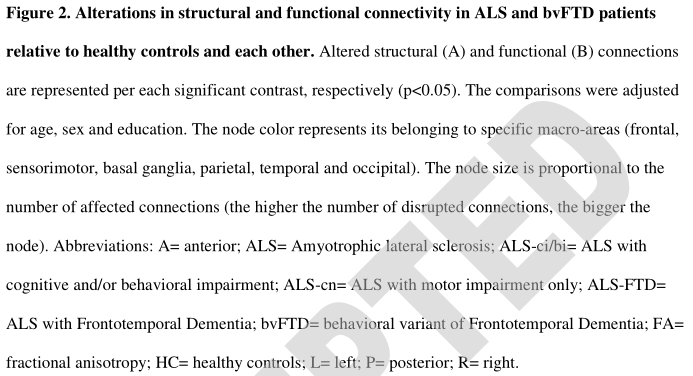
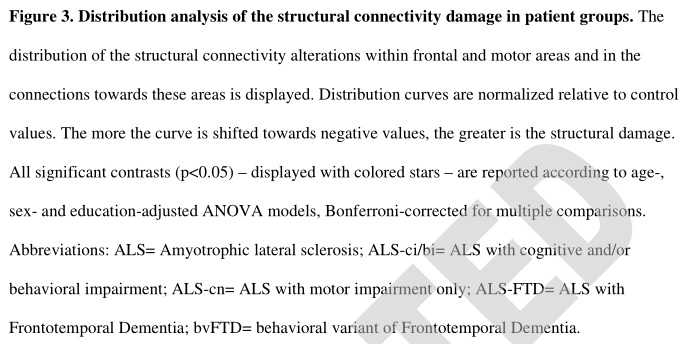
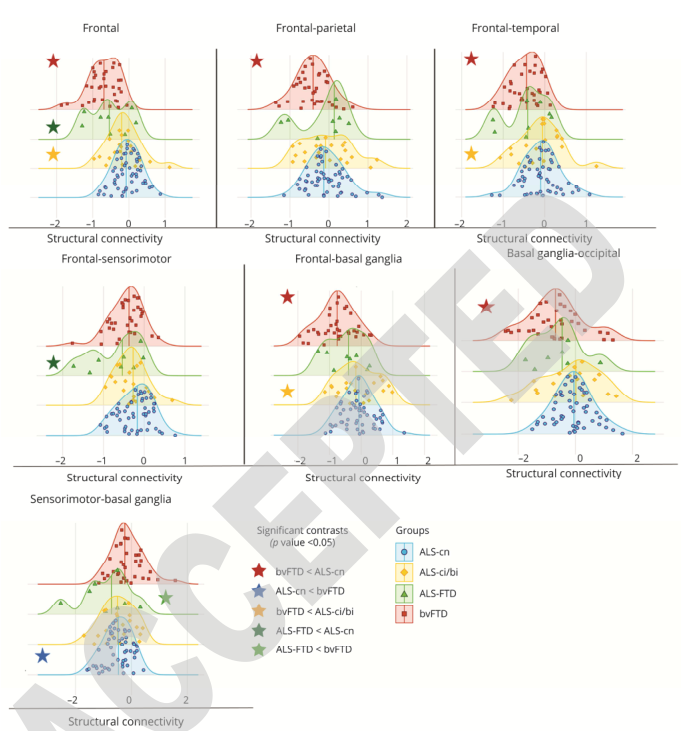
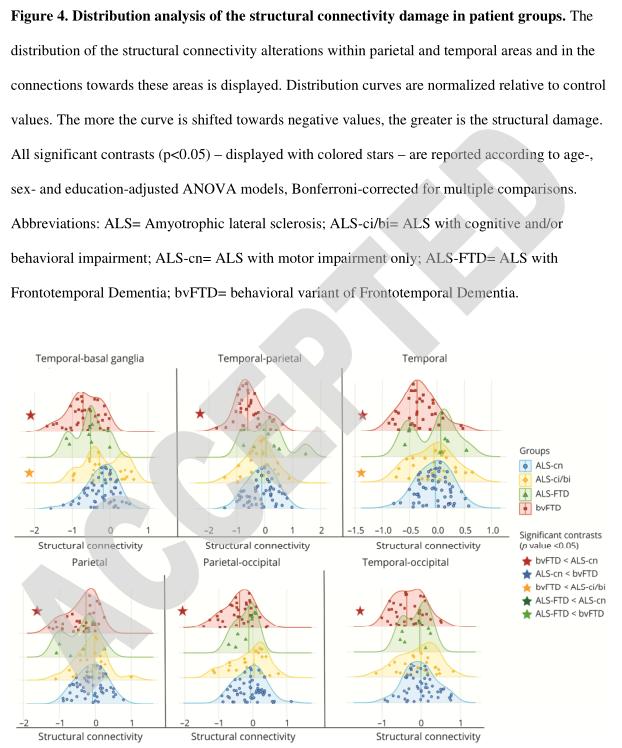
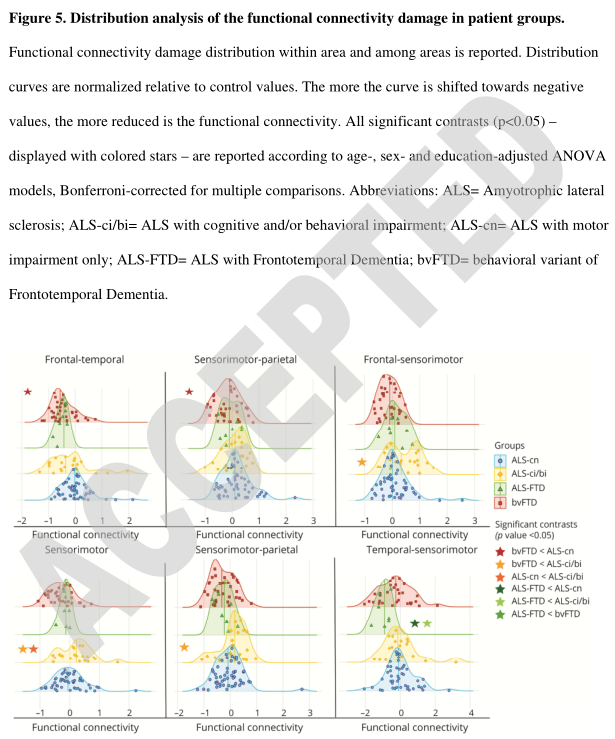
共纳入83名ALS患者,35名BV-FTD患者和61名健康对照,他们接受了临床、认知和MRI评估。ALS患者按修订的STRICE标准分为单纯运动障碍(ALS-CN)54例,认知和/或行为受累(ALS-CI/BI)21例,伴有BV-FTD的ALS(ALS-FTD)8例。首先,评估了ALS-FTD谱的功能和结构连接模式。其次,调查了有任何程度认知障碍(即ALS-CI/BI和ALS-FTD)的ALS患者的MRI连接性改变是否以及在哪里更类似于频谱的一端(ALS-CN)或另一端(BV-FTD)的损害模式,从群体水平转移到单一受试者的分析。
- 与对照组相比,额颞叶和顶叶网络广泛的结构和功能障碍表现为BV-FTD (BV-FTD样型),而感觉运动-基底节区的更局限性结构损害则表现为ALS-CN (ALS-CN样型)。
- 肌萎缩侧索硬化症((ALS-CBI)患者表现出一种“类似ALS-CN”的结构损伤模式,与ALS-CN患者的运动损伤相似,表现为感觉运动区功能连通性增强和功能减退。类似“BV-FTD”模式中的连接性。
- 另一方面,ALS-FTD患者在结构和功能上都类似于BV-FTD样的损害模式,此外,运动区的结构性ALS-CN样损害。
研究发现,与ALS-CN相比,伴有相似结构改变的ALS-CBI的功能重排适应不良,这支持ALS-CI/BI可能被认为是ALS的表型变异,而不是疾病恶化的结果的假说。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Neurol#
34
ALS伴认识和行为损害
65
近日,有研究人员使用MRI连接数据的数学模型来破译ALS-FTD频谱**同的和不同的神经关联。
64
真好
56
学习
67
#变异#
24
#表型#
23