Crit Care:院外心脏骤停成人患者的体外心肺复苏
2022-05-11 MedSci原创 MedSci原创
在这个大队列中,1644例院外心脏骤停患者的体外心肺复苏数据显示出院时神经系统预后良好的比例为14.1%,出院时生存率为27.2%,在体外心肺复苏期间研究人员观察到并发症的比例为32.7%。
体外心肺复苏在世界范围内院外心脏骤停患者中正在迅速流行推广。然而,指南或临床研究并没有提供足够的体外心肺复苏实践数据。
近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,该研究的目的是提供院外心脏骤停患者体外心肺复苏的真实数据,并纳入了并发症情况。
研究人员对日本的观察性多中心队列研究进行了回顾性数据库分析,纳入2013年至2018年期间接受体外心肺复苏的推测为心脏病因的院外心脏骤停成年患者。该研究的主要结局为出院时良好的神经系统结局,定义为1或2级脑功能状态。
该研究共纳入了1644例院外心脏骤停患者。患者平局年龄为18 ~ 93岁,中位数为60岁。现场初始心律中震荡性心律为69.4%。估计的低流量时间中位数为55分钟(四分位差范围:45-66分钟)。14.1%的患者出院时神经系统预后良好,27.2%的患者出院时生存率良好。
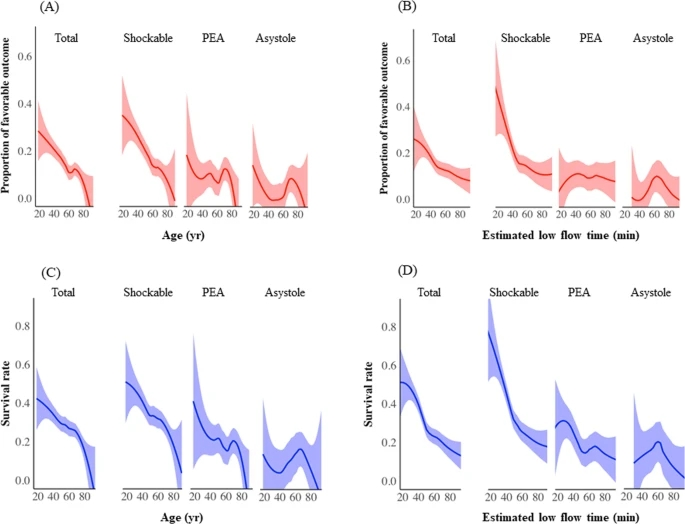
出院时以休克节律、无脉电活动和心搏停止为指标的患者神经系统预后良好的比例分别为16.7%、9.2%和3.9%。32.7%的患者在体外心肺复苏过程中发生并发症,最常见的并发症是出血,其中插管部位出血和其他类型出血的发生率分别为16.4%和8.5%。
由此可见,在这个大队列中,1644例院外心脏骤停患者的体外心肺复苏数据显示出院时神经系统预后良好的比例为14.1%,出院时生存率为27.2%,在体外心肺复苏期间研究人员观察到并发症的比例为32.7%。
原始出处:
Akihiko Inoue,et al.Extracorporeal cardiopulmonary resuscitation in adult patients with out-of-hospital cardiac arrest: a retrospective large cohort multicenter study in Japan.Critical Care.2022.https://ccforum.biomedcentral.com/articles/10.1186/s13054-022-03998-y
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#心肺#
62
#复苏#
54
#院外心脏骤停#
56
#体外心肺复苏#
0