Nat Med:Belzutifan抑制肾细胞癌的I期试验和生物标志物分析
2021-05-03 haibei MedSci原创
在接受每天一次120毫克Belzutifan的ccRCC患者中(n = 55),确认的客观反应率为25%(全部为部分反应),中位无进展生存期为14.5个月。
对肾细胞癌(RCC)分子生物学的进一步了解可以导致治疗方案的实质性发展。目前,对透明细胞肾细胞癌(ccRCC)理解的一个重要进展是Von Hippel-Lindau(VHL)基因在致癌过程中的潜在作用,这反过来又突出了针对相关缺氧反应途径的潜在治疗价值。
VHL基因在大约90%的ccRCC肿瘤中丢失。VHL蛋白(pVHL)有多种功能,但与ccRCC癌变最直接相关的作用是它作为E3泛素连接酶复合物的一个亚单位,介导HIF-2α的蛋白酶体降解。在缺氧条件下,HIF-2α与芳烃受体核易位因子(ARNT,也称为缺氧诱导因子-1β)异源二聚体形成活性转录因子(缺氧诱导因子1),上调缺氧诱导基因的表达,如血管内皮生长因子(VEGF)和红细胞生成素,以对抗缺氧并增加氧合。在正常情况下,HIF-2α上的氧依赖性翻译后修饰使pVHL能够识别并针对HIF-2α进行快速降解。在ccRCC中,pVHL功能的丧失与假性缺氧状态、HIF-2α的积累和下游基因的上调有关。因此,HIF-2α是治疗与pVHL功能障碍相关的肿瘤(如ccRCC)的一个有希望的靶点。
低氧诱导因子-2α(HIF-2α)是一种转录因子,经常在透明细胞肾细胞癌(ccRCC)中积累,导致参与致癌的基因被构成性激活。Belzutifan(MK-6482,以前称为PT2977)是一种有效的、选择性的HIF-2α小分子抑制剂。最近,在一项一期研究(NCT02974738)中,人们首次评估了Belzutifan的最大耐受剂量、安全性、药代动力学、药效学和抗肿瘤活性。该研究入组的患者患有晚期实体瘤(剂量递增组)或以前治疗过的晚期ccRCC(剂量扩展组)。Belzutifan采用3+3的剂量递增设计进行口服,然后在ccRCC患者中以推荐的2期剂量(RP2D)进行扩展。
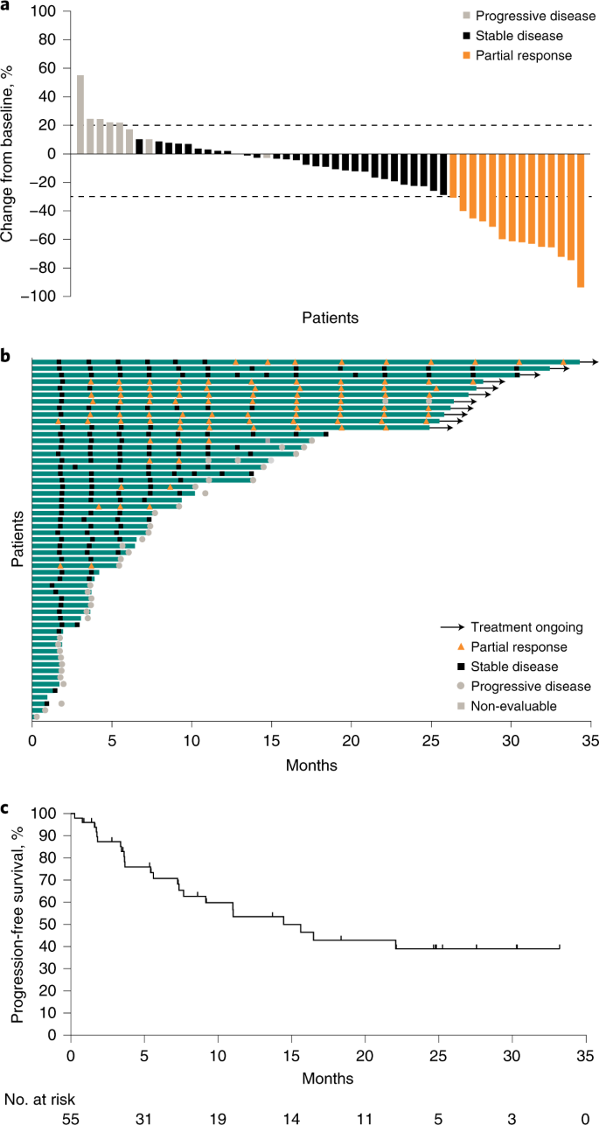
ccRCC队列的疗效结果
在剂量递增队列中(n = 43),在剂量达到160毫克,每天一次的情况下没有发生剂量限制性毒性,也没有达到最大耐受剂量;RP2D为120毫克,每天一次。在所有剂量下都观察到血浆红细胞生成素的减少;红细胞生成素的浓度与belzutifan的血浆浓度相关。
在接受每天一次120毫克Belzutifan的ccRCC患者中(n = 55),确认的客观反应率为25%(全部为部分反应),中位无进展生存期为14.5个月。最常见的≥3级不良事件是贫血(27%)和缺氧(16%)。
因此,该研究表明,Belzutifan耐受性良好,并在大量预处理的患者中表现出初步的抗肿瘤活性,表明HIF-2α抑制可能为ccRCC提供有效的治疗。
原始出处:
Toni K. Choueiri et al. Inhibition of hypoxia-inducible factor-2α in renal cell carcinoma with belzutifan: a phase 1 trial and biomarker analysis. Nature Medicine (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#细胞癌#
32
#标志物#
28
#Nat#
34
#生物标志#
34
#生物标志#
31
#Med#
19