Blood Cells Mol Dis:艾曲波帕作为原发性免疫性血小板减少症患者二线治疗的有效性和安全性
2021-10-31 MedSci原创 MedSci原创
研究证实了艾曲波帕作为二线治疗慢性ITP患者的有效性和安全性
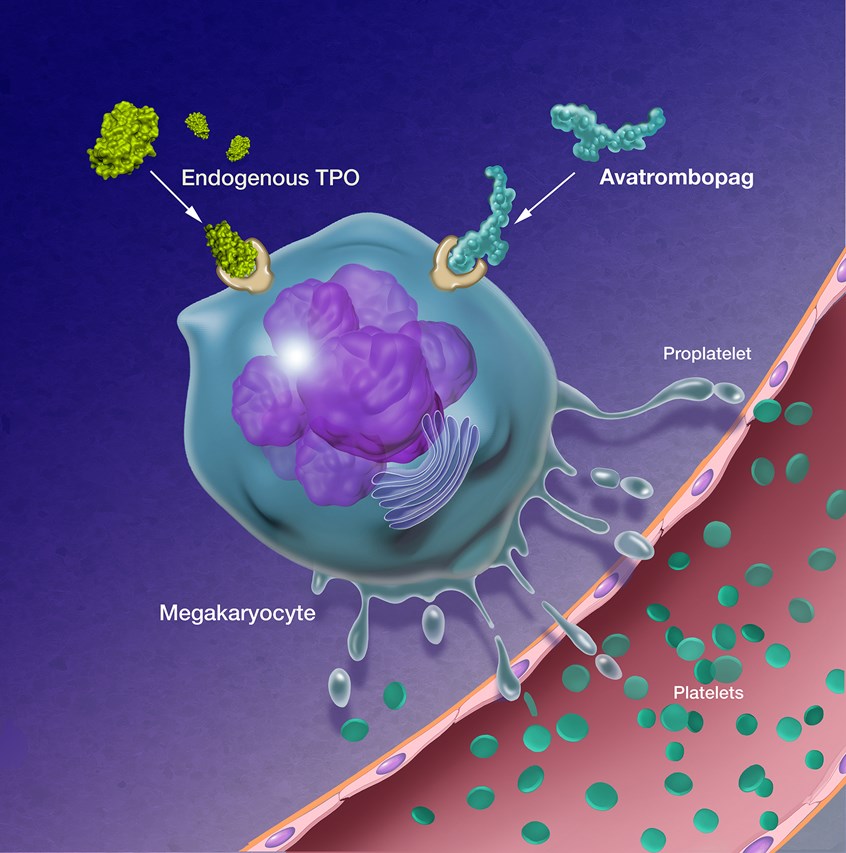
糖皮质激素治疗是免疫性血小板减少症(ITP)患者的标准初始治疗方法。尽管最初的缓解率为60-80%,但只有30-50%的成年人在停药后有持续的反应。二线选择是脾切除术、血小板生成素受体激动剂(TPO-RAs)、利妥昔单抗和静脉注射免疫球蛋白。三线治疗包括混合的免疫抑制药物(如硫唑嘌呤、环孢素等)。
最近,国际指南提出了一种治疗算法,将TPO-RAs和脾切除术分别确定为二线和三线,确认脾切除术仅在紧急情况下作为二线选择。
国外一个研究团队提出了一项单中心观察性回顾性研究,作为二线治疗的方法。自2003年以来,他们评估了48例成人原发性慢性ITP患者。48例患者中有44例接受了糖皮质激素的一线治疗。22例(61%)患者需要二线治疗:18例接受埃特罗巴,3个疗程的类固醇,1例患者接受脾切除术。每个患者在开始切除或接受脾切除术前都接受了骨髓检查。
结果提示艾曲波帕的总有效率率为94%,CR率为76%,PR为23%;只有1例患者无反应,接受脾切除术,随后接受利妥昔单抗、罗米plostim和环孢素治疗获得CR。1例患者在开始TPO-RA约一个月后出现自身免疫性全血细胞减少,除埃尔龙巴格外,还接受类固醇和利妥昔单抗治疗,血计数改善。中位随访时间为21,1个月(范围为0,4,64,7个月),16例患者(89%)仍在治疗中维持应答。安全性方面,胃肠道不良反应少见,级别低;只有一名患者在几周后因头晕而停止使用艾曲波帕。1例患者深静脉血栓复发,无大出血并发症。
综上所述,这次的真实世界单中心实验证实了艾曲波帕作为二线治疗慢性ITP患者的有效性和安全性。
原始出处:
Gardellini A,Guidotti F,Feltri M,et al.Eltrombopag as second line treatment in patients with primary immune thrombocytopenia: A single center real life experience.[J].Blood Cells Mol Dis,1970,:102620.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#原发性#
53
#Dis#
51
#CEL#
49
#Cell#
55
#免疫性血小板减少#
46
#血小板减少#
44
#艾曲波帕#
42
#二线治疗#
52
#cells#
53
很精彩、实用
58