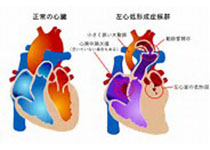
JAHA:扩张型心肌病患儿心率升高与生存率的关系
2020-07-30 MedSci原创 MedSci原创
在扩张型心肌病儿童中,心率升高与死亡和心脏移植的风险增加相关。有必要对扩张型心肌病患儿心率增高与疾病严重程度的关联进行进一步研究,并将其作为潜在的治疗目标。
在心衰成年人,心率升高与生存率降低有关。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在明确扩张型心肌病患儿心率升高是否与死亡或心脏移植风险增加相关。
这项研究是对小儿心肌病登记处的数据进行的分析,包含1994年至2011年期间诊断为扩张型心肌病的557名儿童(51%为男性,中位年龄为1.8岁)的基线数据、年度随访和调查事件(移植或死亡)。升高的心率定义为高于儿童平均心率的2个或更多个SD(根据年龄调整)。该研究的主要结局是心脏移植和死亡。
比起具有正常心率的儿童,年龄较大(中位年龄为2.3岁 vs 0.9岁;P<0.001)的192名儿童(34%)的心率升高,更可能出现心力衰症状(83% vs. 67%;P<0.001),心室功能更差(z值中位数缩短分数,分别为-9.7和-9.1;P=0.02),更有可能接受抗充血治疗(分别为96% vs. 86%;P<0.001)。在控制年龄、心室功能和心脏药物的情况下,升高的心率与死亡(调整后的风险比[HR]为2.6;P<0.001)以及死亡或移植(调整后的HR为1.5;P=0.01)独立相关。
由此可见,在扩张型心肌病儿童中,心率升高与死亡和心脏移植的风险增加相关。有必要对扩张型心肌病患儿心率增高与疾病严重程度的关联进行进一步研究,并将其作为潜在的治疗目标。
原始出处:
Joseph W. Rossano.et al.Elevated Heart Rate and Survival in Children With Dilated Cardiomyopathy: A Multicenter Study From the Pediatric Cardiomyopathy Registry.J AM HEART ASSOC.2020.https://www.ahajournals.org/doi/full/10.1161/JAHA.119.015916
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#扩张#
29
#生存率#
27
#AHA#
41
#肌病#
28
学习了~
77
很受用!
83