Chest:阿奇霉素预防COPD急性加重 超过1年还有效果吗?
2018-06-20 徐钰琦 环球医学
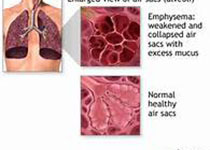
慢性阻塞性肺疾病(COPD)是一种重要的慢性呼吸系统疾病,患者常伴发呼吸困难、缺氧等症状,肺功能会慢慢恶化。病毒引起的上呼吸道感染和肺炎会导致COPD的急性加重(ECOPD),是造成患者突然死亡的主要原因。阿奇霉素作为大环内酯类的抗菌药物,对预防COPD急性加重具有重要作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#急性加重#
22
#Chest#
35
#EST#
24
好文献学习了
52