LANCET:支气管扩张儿童呼吸加重:阿奇霉素非劣效于阿莫西林-克拉维酸?
2018-10-27 吴星 环球医学网
虽然阿莫西林-克拉维酸是推荐的支气管扩张儿童非严重加重的一线经验性口服抗生素治疗药物,但阿奇霉素也因其每天一次给药的便利性而经常使用。2018年10月,发表在《Lancet》的一项多中心、双盲、非劣势、随机对照试探究了在缓解支气管扩张儿童呼吸加重上,阿奇霉素是否非劣效于阿莫西林-克拉维酸。
背景:虽然阿莫西林-克拉维酸是推荐的支气管扩张儿童非严重加重的一线经验性口服抗生素治疗药物,但阿奇霉素也因其每天一次给药的便利性而经常使用。据研究人员所知,还没有发表过纳入支气管扩张急性加重的儿童的随机对照试验。研究人员假设,在缓解支气管扩张儿童呼吸加重上,阿奇霉素非劣效于阿莫西林-克拉维酸。
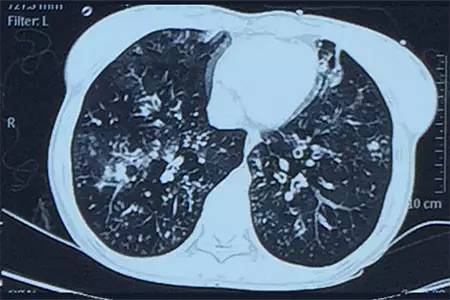
方法:2012年4月~2016年8月,研究人员在3家澳大利亚医院和1家新西兰医院进行了一项平行组、双模拟、双盲、非劣效性随机对照试验。纳入的患儿为影像学证实与囊性纤维化不相关的1~19岁的支气管扩张儿童。加重开始时,儿童随机分配到阿莫西林-克拉维酸(22.5mg/kg,每天两次)+安慰剂或阿奇霉素(5 mg/kg,每天一次)+安慰剂的口服悬浮液,共治疗21天。研究人员使用具有分配隐藏的置换块随机化(根据年龄、地区和病因分层)。首要结局指标为按方案执行人群21天时加重的缓解(定义为回到基线),非劣效性界值为-20%。研究人员评估了数个次要结局,包括加重持续时间、下一次加重的时间、实验室、呼吸、生活质量测量和微生物学。
结果:研究人员筛查了604名儿童,入组了236人。179名儿童加重并分配到治疗组中,阿莫西林-克拉维酸组97人,阿奇霉素组82人。21天时,阿奇霉素组有61/73例(84%)加重缓解,阿莫西林-克拉维酸组为73/87例(84%)。风险差表明非劣效性(-0.3%;95% CI,-11.8~11.1)。阿莫西林-克拉维酸组比阿奇霉素组加重的持续时间显着性短(中位10天(IQR,6~15)vs 14天(8~16);P=0.014)。因治疗药物而造成的不良事件分别为,阿奇霉素组17/82人(21%),阿莫西林-克拉维酸组23/97人(24%)(相对风险,0.9;95% CI,0.5~1.5)。
结论:治疗21天时,在缓解非严重支气管扩张儿童呼吸加重上,阿奇霉素非劣效于阿莫西林-克拉维酸。一些患者中,如青霉素超敏反应或可能具有较差依从性的患者,阿奇霉素是治疗加重的替代选择,但是必须平衡治疗失败风险(20%的界值内)、更长的加重时间和诱导大环内酯类耐药风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#克拉维酸#
35
#支气管#
35
#扩张#
35
#Lancet#
35
#非劣效#
33