CELL STEM CELL:PAPD5小分子抑制剂恢复干细胞中端粒酶活性
2020-05-03 MedSci原创 MedSci原创
降低端粒酶活性的遗传性病变会抑制干细胞的复制,导致一系列不治之症,包括先天性皮肤病(DC)和肺纤维化(PF)。
降低端粒酶活性的遗传性病变会抑制干细胞的复制,导致一系列不治之症,包括先天性皮肤病(DC)和肺纤维化(PF)。
至今为止,如何恢复全身干细胞中端粒酶的活性仍不清楚。
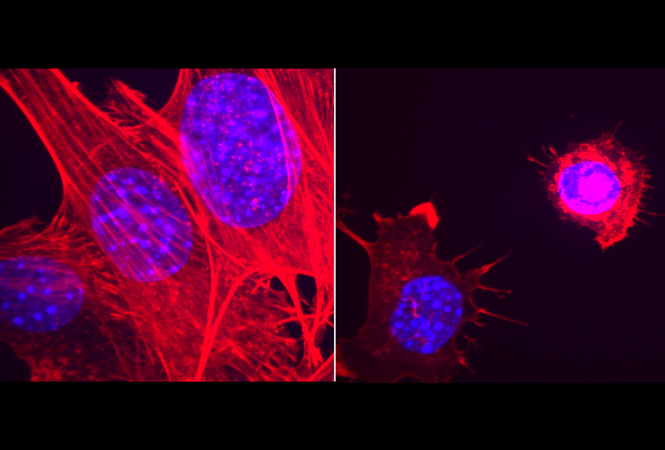
最近,研究人员发现,PAPD5的小分子抑制剂能够在体外、干细胞模型和体内帮助端粒恢复。
PAPD5是一种非典型的聚合酶,可低聚腺苷酸化,并破坏端粒酶RNA组分(TERC)的稳定。研究人员发现了小分子BCH001,一种特异性的PAPD5抑制剂,可以在DC患者诱导的多能干细胞中恢复端粒酶活性和端粒长度。
当研究人员将工程化的携带DC致病PARN突变的人类血液干细胞异种移植到免疫缺陷小鼠体内时,口服PAPD5抑制剂二氢喹嗪酮RG7834,可恢复TERC 3'成熟和端粒长度。
这些发现为开发系统性的端粒治疗药物,以对抗DC、PF,以及其他衰老相关疾病的干细胞衰竭提供了策略。
原始出处:
Nagpal N et al. Small-Molecule PAPD5 Inhibitors Restore Telomerase Activity in Patient Stem Cells. CELL STEM CELL (2020). doi: 10.1016/j.stem.2020.03.016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













已拜读,受益匪浅。
39
#小分子抑制剂#
52
#小分子#
43
#PAP#
51
#抑制剂#
48
#CEL#
20
#stem cell#
36
#Cell#
40
#端粒酶活性#
34
干细胞是热点,但是进入临床仍然需要时间和临床疗效验证哦
48