双侧股骨干骨折行髓内钉固定,同期还是分期手术?
2021-11-08 网络 网络
一项多中心研究比较了双侧股骨干骨折,同期固定与分期固定在并发症方面的差异。结果是同期双侧股骨髓内钉固定可降低可耐受确定性手术的多发伤患者ARDS的发生率。
对股骨干骨折,髓内钉固定已成标注术式。但双侧股骨干骨折髓内钉的内固定治疗,双侧应同期固定或分期固定,仍存争议。同期固定可避免二次手术风险,但手术创伤大,对严重创伤患者存在“二次打击”,可能会导致不良结局并发症发生。
对此,一项多中心研究比较了双侧股骨干骨折,同期固定与分期固定在并发症方面的差异。文章发表于2021.09 JOT杂志。

Objective(目的)
评价髓内钉(IMN)治疗双侧股骨骨折患者在同期手术或2次分期手术中的并发症发生率。
[Objective: To evaluate rates of complications in patients with bilateral femur fractures treated with intramedullary nailing (IMN) during either 1 single procedure or 2 separate procedures.]
Patients(病例)
10个一级创伤中心对自1998年至2018年间接受同期单次或两次分期手术治疗的双侧股骨骨折患者进行了多中心回顾性研究。共纳入246例双侧股骨骨折患者。
[Patients: A multicenter retrospective review of patients sustaining bilateral femur fractures, treated with IMN in single or 2-stage procedure, from 1998 to 2018 was performed at 10 Level-1 trauma centers. Two hundred forty-six patients with bilateral femur fractures.]
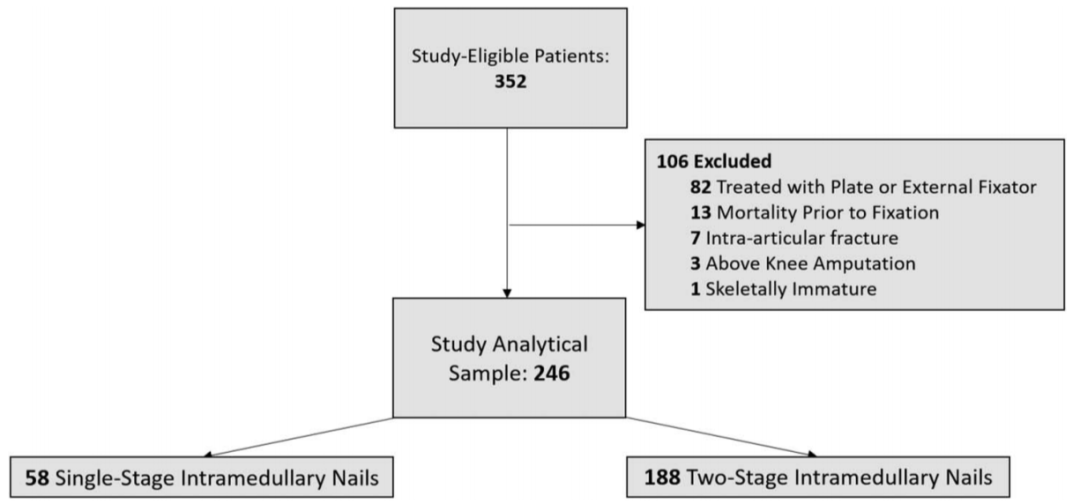
图1 病例挑选与治疗方法流程图。
Results(结果)
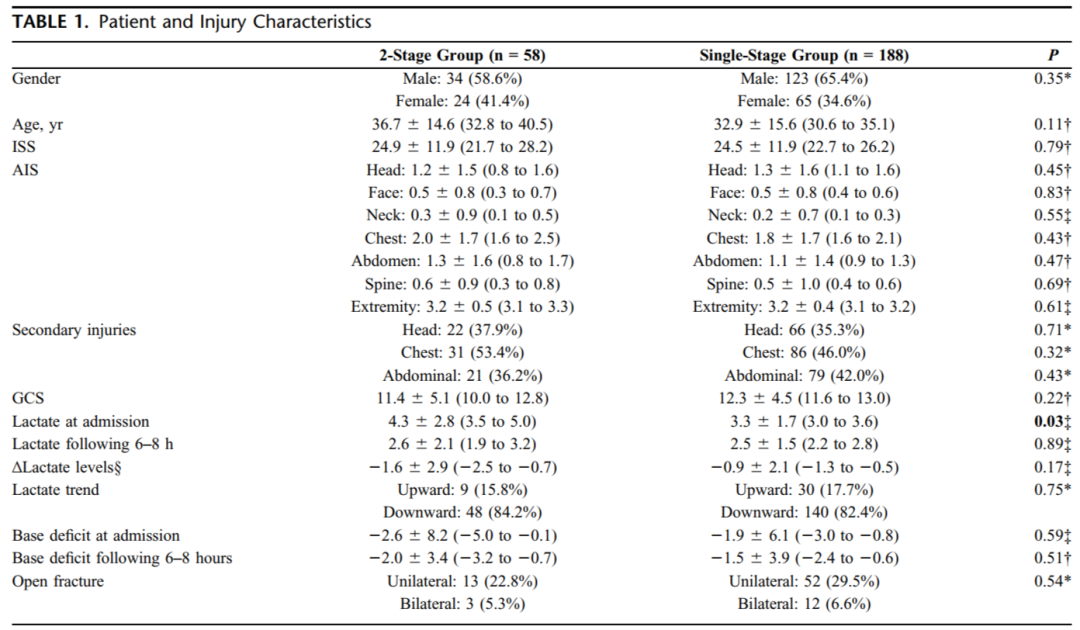
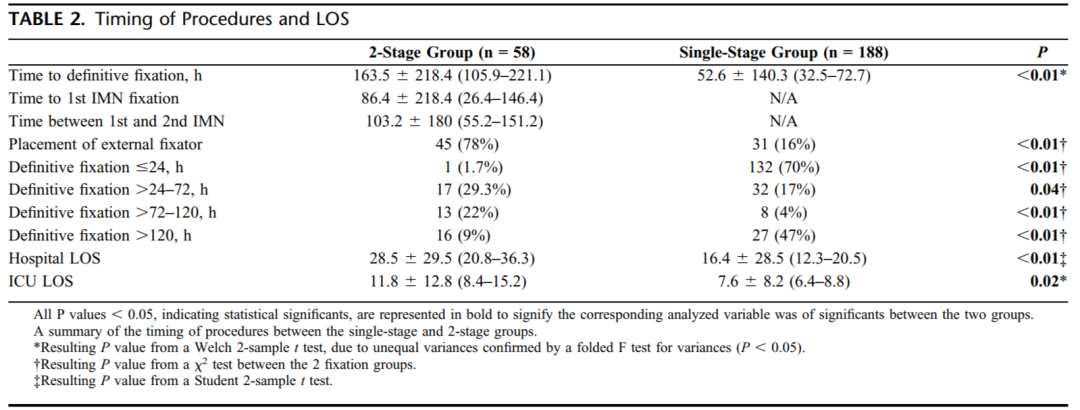
[Results: A total of 246 patients were included, with 188 singlestage and 58 two-stage patients. Gender, age, injury severity score, abbreviated injury score, secondary injuries, Glasgow coma scale, and proportion of open fractures were similar between both groups. Acute respiratory distress syndrome (ARDS) occurred at higher rates in the 2-stage group (13.8% vs. 5.9%; P value = 0.05). When further adjusted for age, gender, injury severity score, abbreviated injury score, Glasgow coma scale, and admission lactate, the single-stage group had a 78% reduced risk for ARDS. In-hospital mortality was higher in the single-stage cohort (2.7% compared with 0%), although this did not meet statistical significance (P = 0.22).]
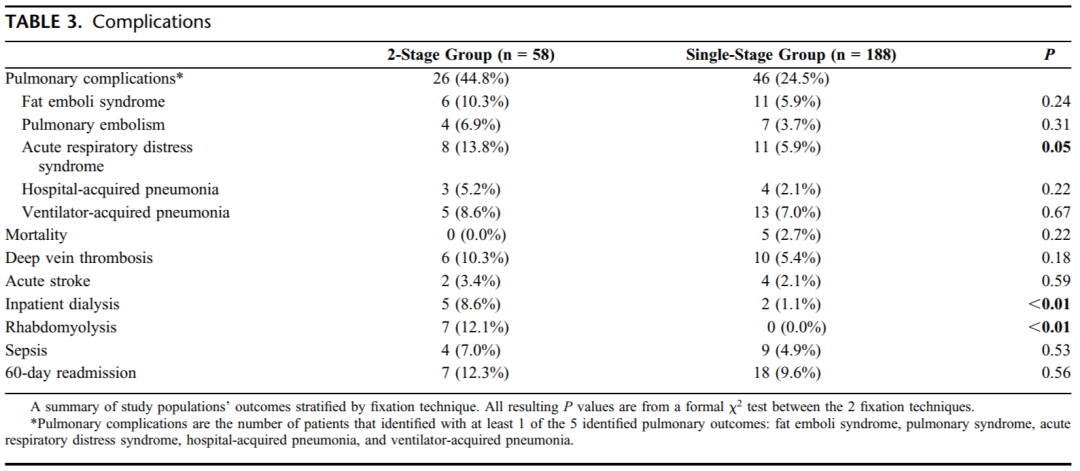
Conclusion(结论)
[Conclusion: This is the largest multicenter study to date evaluating the outcomes between single- and 2-stage IMN fixation for bilateral femoral shaft fractures. Single-stage bilateral femur IMN may decrease rates of ARDS in polytrauma patients who are able to undergo simultaneous definitive fixation. However, a future prospective study with standardized protocols in place will be required to discern whether single- versus 2-stage fixation has an effect on mortality and to identify those individuals at risk.]

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#股骨干#
50
#骨干骨折#
30
#髓内钉固定#
38
#同期#
37
#髓内钉#
44
#双侧#
28
#股骨#
39