III期ADAURA试验:Tagrisso在EGFR突变型肺癌患者的辅助治疗中具有压倒性疗效
2020-04-11 Allan MedSci原创
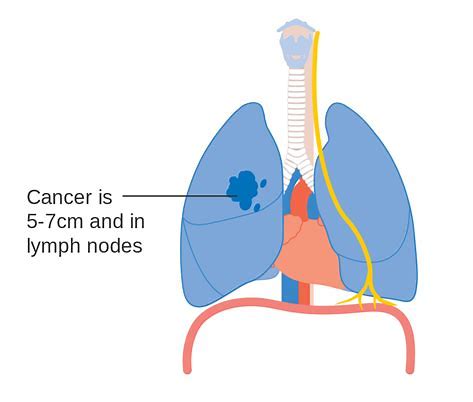
III期ADAURA临床试验显示,Tagrisso(osimertinib)在辅助治疗IB、II和IIIA期表皮生长因子受体突变(EGFRm)非小细胞肺癌(NSCLC)且肿瘤完整切除的患者具有显著疗效
III期ADAURA临床试验显示,Tagrisso(osimertinib)在辅助治疗IB、II和IIIA期表皮生长因子受体突变(EGFRm)非小细胞肺癌(NSCLC)且肿瘤完整切除的患者具有压倒性疗效。因此,独立数据监察委员会(IDMC)建议提前终止III期ADAURA试验。
阿斯利康肿瘤学研究与开发执行副总裁José Baselga表示:“我们对提前结束ADAURA III期临床试验感到很高兴。非小细胞肺癌是一种灾难性的肿瘤,EGFR靶向药物现在首次可以提供治愈的希望”。
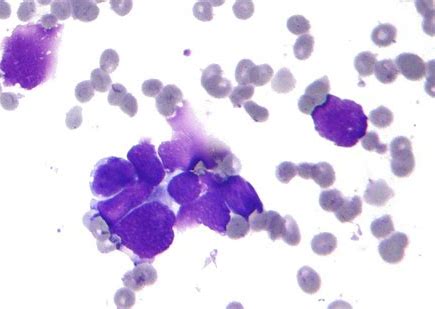
根据在显微镜下的外观,肺癌可以分为两大类:小细胞肺癌(small cell lung cancer)和非小细胞肺癌(non small cell lung cancer)。非小细胞肺癌更为常见,目前约占肺癌病例的87%。非小细胞型肺癌包括鳞状细胞癌(鳞癌)、腺癌、大细胞癌,与小细胞癌相比其癌细胞生长分裂较慢,扩散转移相对较晚。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#III#
23
#压倒性疗效#
30
#突变型#
25
#肺癌患者#
24
#ADA#
35
#Tagrisso#
24
#GFR#
17
#III期#
28
谢谢梅斯提供这么好的信息,学到很多
51