Liver Cancer:卡博替尼(Cabozantinib)治疗晚期肝癌的疗效和安全性:来自国际多中心真实世界研究
2021-06-02 yd2015 MedSci原创
卡博替尼(Cabozantinib)治疗晚期肝癌是有效、安全、可行的措施。
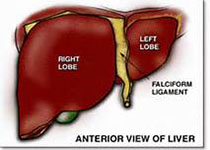
肝细胞癌(HCC)是常见的恶性肿瘤。对于晚期HCC,长期以索拉非尼为标准一线治疗。近3年来,相继出现仑伐替尼一线治疗非劣效于索拉非尼,而PDL1抑制剂阿替利珠单抗联合贝伐珠单抗一线治疗优于索拉非尼。而对于二线以及后线治疗中,有瑞戈非尼、雷莫芦单抗和卡博替尼(Cabozantinib)等药物。我们都知道,基于临床研究的结果并不能真实反应药物的疗效和安全性,因为临床研究有着严格的入组和排除标准,但是真实世界中很多并不能达到这些标准。而目前对于卡博替尼来说,还没有大型的真实世界研究来评估其疗效和安全性。因此,来自澳大利亚、瑞士和德国的研究团队开展了一项真实世界回顾性研究,评估卡博替尼治疗晚期肝癌的疗效和安全性。研究成果发表在Liver Cancer杂志上。
该研究回顾性纳入澳大利亚、瑞士和德国三个国家11个研究中心的晚期肝癌患者,收集患者的临床特征、治疗不良事件、治疗持续时间和总生存期(OS)。研究共纳入了88利患者,76例患者 (86%)为男性,中位年龄为66岁(range 25–84岁)。26例患者 (30%)伴有非酒精性肝炎,而21例患者(24%)伴有丙肝感染。78例患者(89%)为巴塞罗那分期(BCLC)C期。大多数患者 (n = 60, 68%) 肝功能评级为Child-Pugh stage A, 22例患者 (25%) 为Child-Pugh stage B,1例患者(1%) 为Child-Pugh stage C, 其他5例患者没有报道。
81例患者 (92%) 在卡博替尼治疗前接受过索拉非尼。28例患者(32%)卡博替尼治疗前用过2线系统治疗和15例(17%)患者使用过3线治疗。3名患者(3%)甚至使用过4线治疗。52名患者(59%)在随访中死亡。卡博替尼治疗开始的中位随访时间为4.8个月(范围:0.7 -18.4个月)。
疗效评估,6例患者(7%) 达到部分缓解 (PR), 28例患者(32%) 达到稳定, 28例患者(32%) 出现疾病进展(PD)。卡博替尼开始治疗的总体人群中的中位OS为210天(7.0个月) (95% CI 150–269天),中位PFS为102天 (3.4个月)(95% CI 82–121 days)。
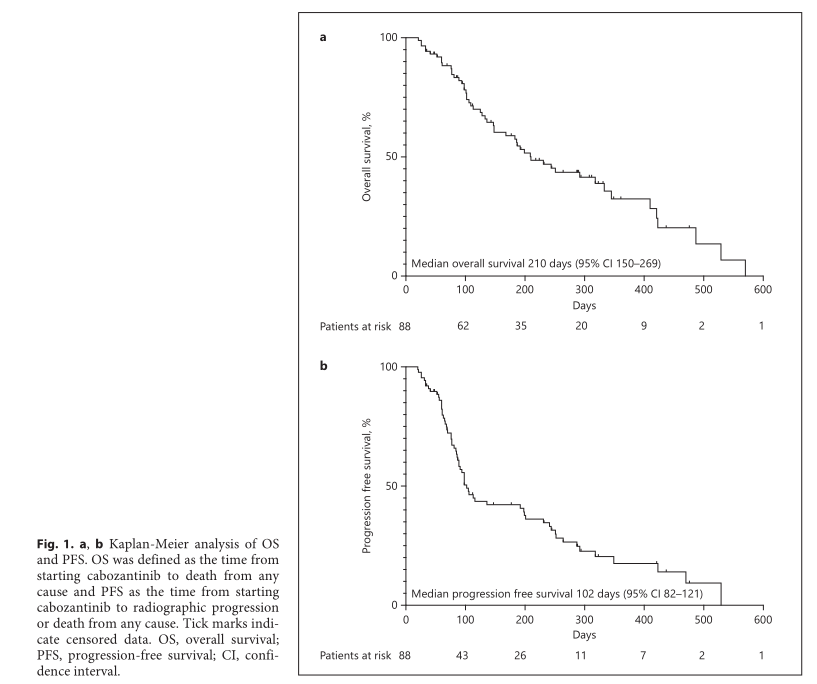
卡博替尼治疗总体人群的OS和PFS
对于达到PR和稳定的患者,中位OS为423天,而PD患者的中位 OS为187天(HR=2.349,95%CI 1.1457–4.817,p = 0.007)。
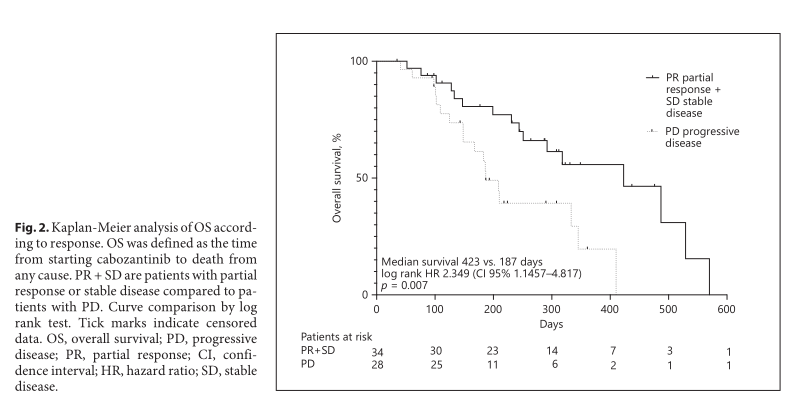
不同治疗应答患者的OS
Child-Pugh A 患者的中位OS为9.7个月,Child-Pugh B患者的中位OS为3.4个月,两组有统计学差异(HR=3.0, 95%CI 1.316–7.010, P=0.01)。 Child-Pugh A和B患者的PFS分别为98天(79–116) 和 94天(73–114)。37例患者(42%) 符合CELESTIAL临床研究标准的患者,其中位OS为11.1个月。

Child-Pugh A和B患者的OS
45例患者(51%)报道了至少一种不良事件 (AE)。最常见的不良事件为疲劳(16.5%),腹泻 (16.5%)和食欲下降(11%)。
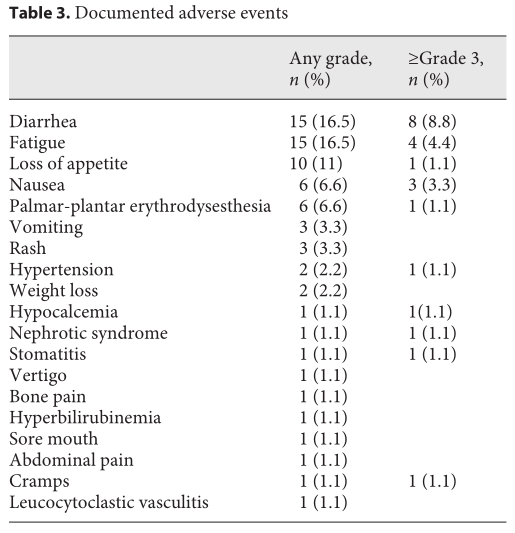
治疗常见不良反应
综上,卡博替尼(Cabozantinib)治疗晚期肝癌是有效、安全、可行的措施。
原始出处:
Fabian Finkelmeier, Bernhard Scheiner, Catherine Leyh, et al. Cabozantinib in Advanced Hepatocellular Carcinoma: Efficacy and Safety Data from an International Multicenter Real-Life Cohort. Liver Cancer. 2021. DOI: 10.1159/000515490. Published online: June 1, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疗效和安全性#
30
#多中心#
27
受教了 谢谢
60
#真实世界#
37
#cabozantinib#
34
#ABO#
29
谢谢梅斯提供这么好的信息,学到很多
45
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
42