Bosworth骨折脱位,可否合并后踝骨折?
2021-12-08 Dr. Zhang 骨科青年
有学者汇报了一组Bosworth骨折病例,并回顾相关文献,以研究Bosworth骨折合并后踝骨折的几率。
Bosworth骨折由美国医生David Marsh Bosworth于1947年首先报道,其特点是外旋暴力导致踝关节骨折脱位,伴腓骨近端骨折移位、交锁于胫骨后嵴处。因骨间膜、韧带及腓骨肌腱被拉紧,闭合手法复位比较困难,常需手术切开复位。为少见的踝关节骨折脱位。
Bosworth骨折通常伴有外踝下胫腓韧带水平的骨折,腓骨交锁、脱位后,外旋暴力是否持续导致后踝骨折?而后踝骨折的存在与否,则与踝关节骨折预后息息相关。
为此,有学者汇报了一组Bosworth骨折病例,并回顾相关文献,以研究Bosworth骨折合并后踝骨折的几率。



Objectives(目的)
[Objectives: Posterior malleolar fractures (PM) have been linked to inferior outcome in malleolar fractures. This study aims to analyze the prevalence and pathoanatomy of PM fractures in Bosworth fracturedislocations (BF).]
Material and Methods(病例与方法)

图1 典型Bosworth骨折病例。
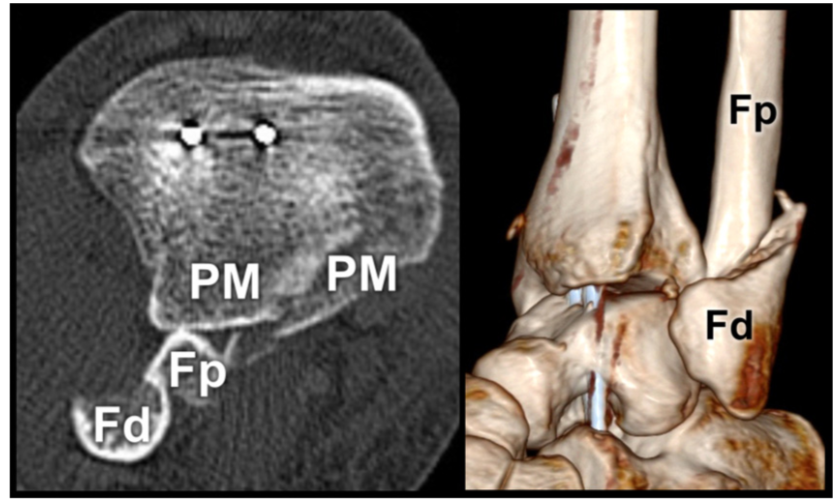
图2 移位的腓骨骨折合并无移位的后踝骨折。
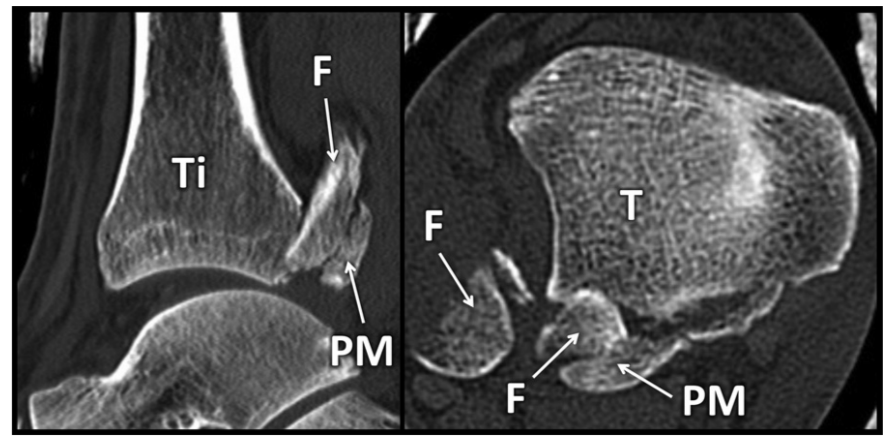
图3 移位的腓骨骨块位于胫骨后侧与后踝骨块之间。
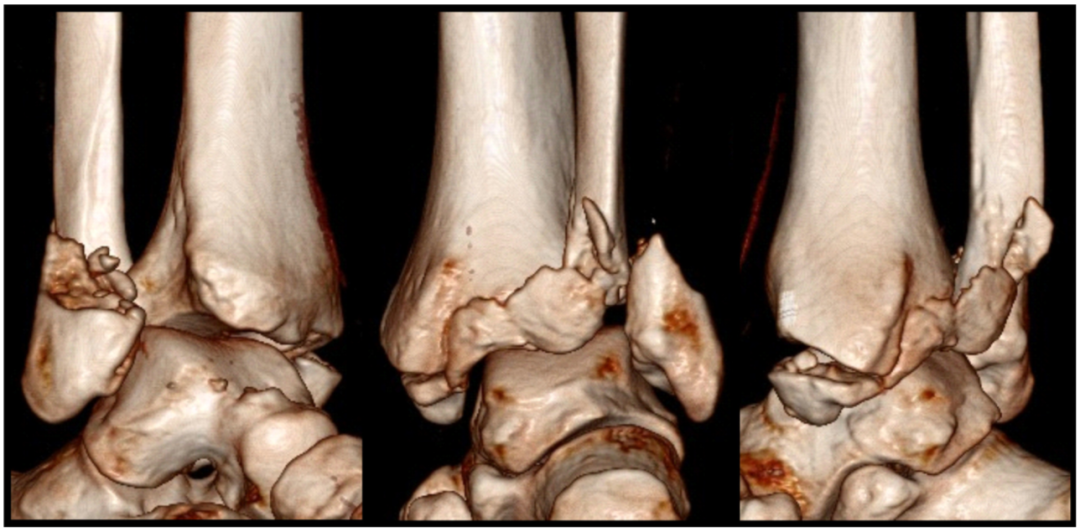
图4 图1X线平片患者的三维重建。可见后踝骨块向内侧延伸。
Results(结果)
本系列的所有13名Bosworth骨折患者(100%)和文献记载的97例中的61例(63%)均与后踝骨折相关。在有完整CT分析的患者中,胫骨后缘后腓骨脱位与切迹外(bartony cek/Rammelt 1型)后踝骨折相关。移位的后踝骨块和胫骨之间的腓骨移位与bartony cek/Rammelt 2型和3型后踝骨折相关。
[Results: All 13 patients (100%) with BF from the present series and 61 of 97 documented cases (63%) of BF from the literature were associated with a PM fracture. In patients with a complete CT analysis, dislocation of the fibula behind the posterior tibial rim was associated with extraincisural (Bartonícek ˇ / Rammelt type 1) PM fracures. Displacement of the fibula between the displaced PM fragment and the tibia was associated with Bartonícek ˇ / Rammelt types 2 and 3 PM fractures.]
Conclusion(结论)

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







好
35
顶
45
#脱位#
36
好文章,值得一读。
37