Cardiovasc Diabetol:钠-葡萄糖共转运体抑制剂对CVD患者心血管、肾脏和安全预后的影响
2021-05-04 Nebula MedSci原创
SGLT-2i对心血管结局有显著的临床疗效,对急性肾损伤也有明显的影响
对照研究和观察性研究表明,2型钠-葡萄糖共转运体抑制剂(SGLT-2i)有利于心力衰竭(HF)患者的生存预后。然而,目前尚不清楚SGLT-2i是否能为患有其他心血管疾病的患者提供益处。
该研究是一项系统回顾和荟萃分析,旨在确定心血管疾病患者应用SGLT-2i对其心血管、肾脏和安全性预后的影响。
研究人员检索了PubMed、EMBASE、Cochrane Library、Web of Science和ClinicalTrials.gov数据库,筛选了从最初到2020年11月1日期间的随机对照试验。两位审查员独立鉴定随机对照试验,比较了SGLT-2i对患有或不患有糖尿病的心血管疾病患者的疗效。主要结果是心血管预后和肾脏预后。次要结果是安全预后,包括不良内分泌结局和不良感染结局。
筛选了10个随机对照试验,共涵盖了25108名SGLT-2i组患者和18574名安慰剂组患者。
两组患者的全因死亡率
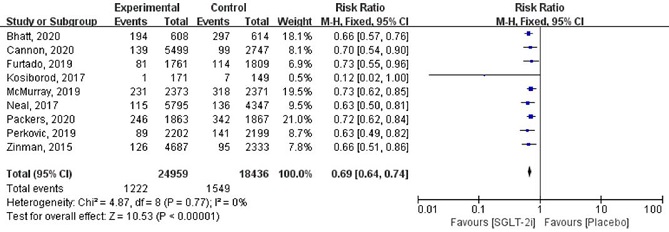
Meta分析显示,SGLT-2i治疗显著降低了心血管疾病患者的全因死亡率、心血管死亡率和心力衰竭住院时间(HHF)(全因死亡率相对危险比[RR]:0.86;95%CI 0.81-0.91;P<0.00001;I2=?0%;心血管死亡率RR:0.85;95%CI 0.79-0.92;P<0.0001;I2=?26%;HHF RR:0.69;95%CI 0.64-0.81;P<0.00001;I2=?0%)。
两组患者的HHF风险
在HF患者中,射血分数降低的HF患者在SGLT-2I治疗后的死亡率和HHF显著降低/减少,而射血分数不变的HF患者与安慰剂治疗相比没有明显差别。
此外,SGLT-2i诱导的肾损伤和心肌梗死的发生率低于安慰剂组,但感染、截肢、容量耗竭和糖尿病酮症酸中毒的风险较高。
综上,SGLT-2i对心血管结局有显著的临床疗效,对急性肾损伤也有明显的影响。SGLT-2i对心血管疾病的影响与有无糖尿病无关。
原始出处:
Zheng, C., Lin, M., Chen, Y. et al. Effects of sodium‐glucose cotransporter type 2 inhibitors on cardiovascular, renal, and safety outcomes in patients with cardiovascular disease: a meta‐analysis of randomized controlled trials. Cardiovasc Diabetol 20, 83 (2021). https://doi.org/10.1186/s12933-021-01272-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ASC#
29
#转运#
42
#抑制剂#
33
#BET#
33
#DIA#
31
谢谢分享!
61