抗CD38抗体-药物偶联物(ADC)STI-6129治疗淀粉样变性:FDA已批准IND
2020-05-27 Allan MedSci原创
Sorrento制药公司今日宣布,美国FDA已批准STI-6129治疗淀粉样变性的研究性新药申请(IND)。
Sorrento制药公司今日宣布,美国FDA已批准STI-6129治疗淀粉样变性的研究性新药申请(IND)。STI-6129融合了多种技术:从G-MAB™抗体文库中鉴定出的全人源抗CD38特异性抗体及位点特异性C-LOCK偶联技术。
Sorrento Therapeutics董事长兼首席执行官Henry Ji博士说:“STI-6129将与我们的CD38 CAR-T计划一起,有望成为淀粉样变性患者的治疗选择。我们期待在临床试验中进一步评估STI-6129的安全性和有效性”。Sorrento打算在晚期复发和/或难治性全身性淀粉样变性患者中启动I期多中心、开放标签、剂量递增的临床试验,其主要目的是确定STI-6129的安全性、初步疗效和药代动力学特征。
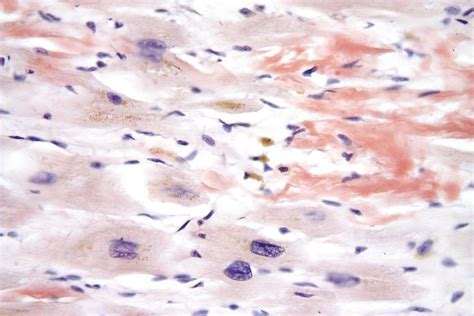
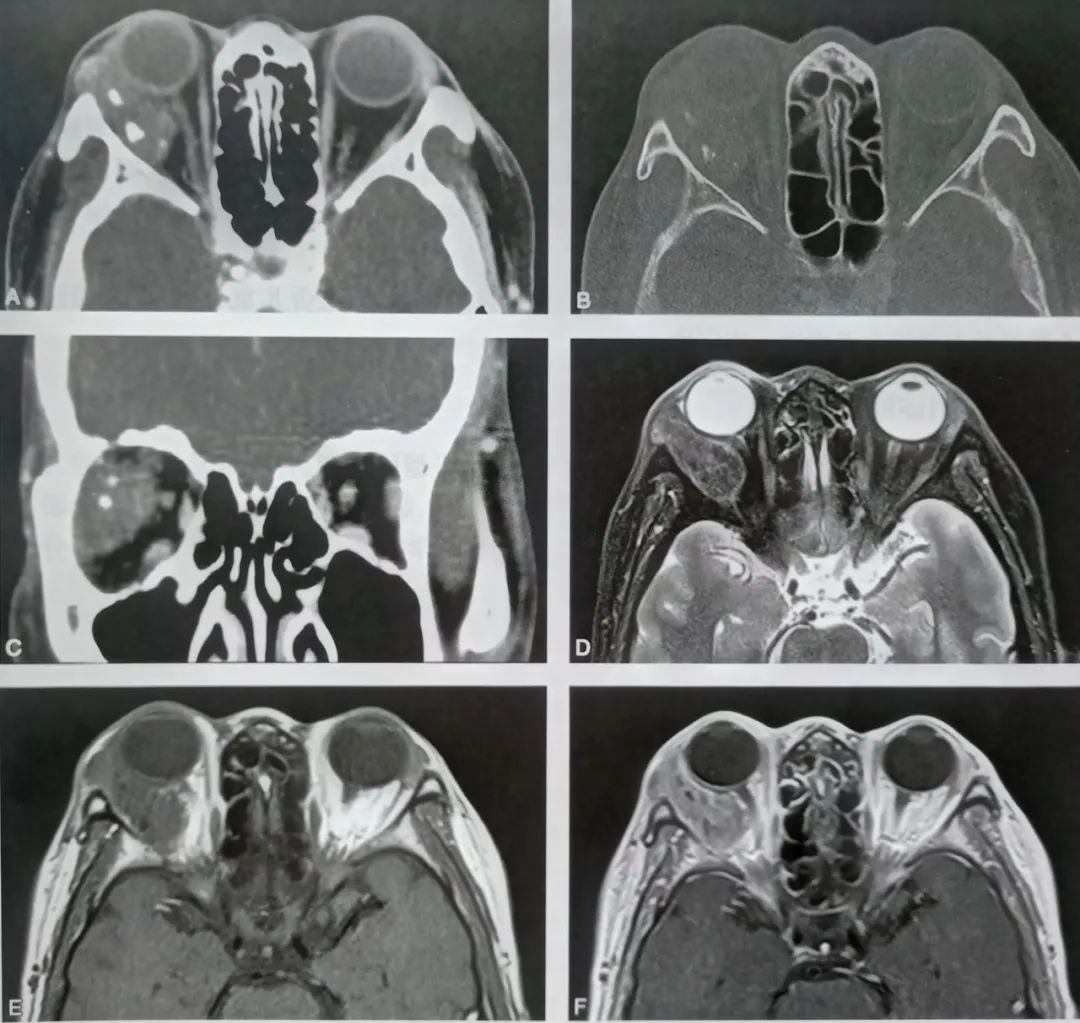
淀粉样变性是一个通用术语,用来指由各种蛋白质的低分子量亚单位组成的原纤维在细胞外组织发生沉积,这些蛋白质大多作为血浆成分进行循环。这些沉积物可能会导致许多不同的临床表现,这取决于沉积物的类型、沉积部位和沉积量。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#STI-6129#
18
#抗体-药物偶联物#
45
#淀粉样变#
25
#淀粉样变性#
30
#变性#
23
#IND#
31