JAHA:外周微血管内皮功能障碍对白质高信号的影响
2021-10-10 MedSci原创 MedSci原创
外周内皮功能障碍与50岁以上患者皮质旁WMH体积增加有关,这是预测未来IS风险的潜在标志。
白质高信号(WMH)以T2加权液体衰减反转恢复脑磁共振成像高信号为特征,与缺血性卒中(IS)风险增加有关。内皮功能障碍是血管功能障碍的指标,可预测IS风险。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在调查内皮功能障碍与区域WMH之间的关联,及其对未来IS风险的影响。
研究人员招募了219名患者(平均年龄为53.1±14.1岁;34.7%为男性),他们使用反应性充血外周动脉眼压计和脑磁共振成像进行了外周内皮功能评估,没有任何IS病史。
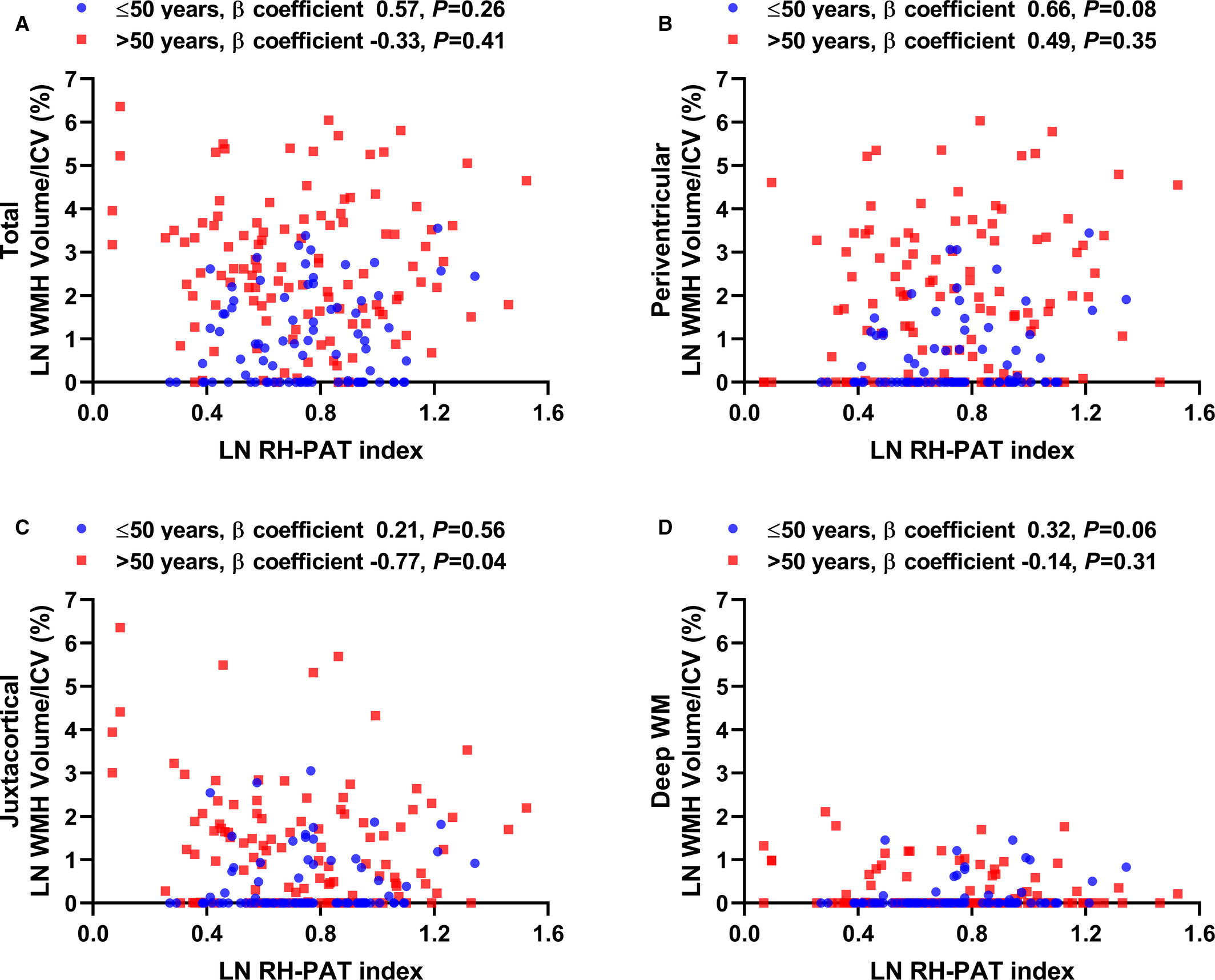
总体和皮质附近WMH体积/颅内体积(%)随着年龄的增长而增加,并且在50岁以上的患者(n=131)中比50岁以下的患者(n=88)更为突出(总WMH:≤50岁,Pearsonr=0.24,P=0.03;>50岁,Pearsonr=0.62,P<0.0001;近皮质WMH:≤50岁,Pearsonr=0.09,P=0.40;>50岁,Pearsonr=0.55,P<0.0001)。在调整其他协变量后,反应性充血外周动脉张力测量指数与总体和皮质旁WMH体积/颅内体积(%)呈负相关(反应性充血外周动脉张力测量指数,标准化β系数为-0.17,P=0.04)。在中位随访6.5年期间,皮质旁WMH体积/颅内体积(%)与IS风险增加相关(风险比为1.47;95%CI为1.05-1.92;P=0.03)。
由此可见,外周内皮功能障碍与50岁以上患者皮质旁WMH体积增加有关,这是预测未来IS风险的潜在标志。
原始出处:
Takumi Toya.et al.Impact of Peripheral Microvascular Endothelial Dysfunction on White Matter Hyperintensity.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.021066
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#内皮功能障碍#
37
#血管内皮功能障碍#
33
#高信号#
0
#血管内皮功能#
0
#白质#
29
#AHA#
29
#微血管#
26
#白质高信号#
34
#功能障碍#
33
#内皮功能#
49