Blood:HO-1hi循环单核细胞可降低镰刀细胞病患者发生血管闭塞的风险
2018-02-04 MedSci MedSci原创
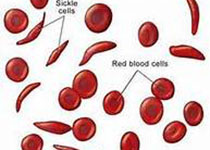
镰状细胞病(SCD)患者常发生与小鼠模型的血管损伤和功能障碍相关的血管内溶性,以及疼痛的血管闭塞危险(VOC),包括镰刀型红细胞黏附增多、激活的淋巴细胞聚集在损伤的血管内皮。在正常情况下,循环中的单核细胞可清除血液循环中受损伤的细胞和碎片,表达较高水平的抗炎血红素氧合酶1(HO-1,血红色降解酶)。现研究人员发现表达HO-1的循环单核细胞可保护SCD血管结构不受持续性溶血损伤和血管闭塞。平均SCD
镰状细胞病(SCD)患者常发生与小鼠模型的血管损伤和功能障碍相关的血管内溶性,以及疼痛的血管闭塞危险(VOC),包括镰刀型红细胞黏附增多、激活的淋巴细胞聚集在损伤的血管内皮。在正常情况下,循环中的单核细胞可清除血液循环中受损伤的细胞和碎片,表达较高水平的抗炎血红素氧合酶1(HO-1,血红色降解酶)。
现研究人员发现表达HO-1的循环单核细胞可保护SCD血管结构不受持续性溶血损伤和血管闭塞。平均SCD患者37%的循环单核细胞可表达较高水平的HO-1(HO-1hi),而健康对照人群中仅有6%,表明HO-1hi表达依赖于对血管内皮细胞的吸收。近期发生过节段性VOC的SCD患者HO-1hi的循环单核细胞的数量降低。
通过小鼠SCD红细胞(RBCs)的亚铁红素介导的血管闭塞在缺乏循环单核细胞的小鼠中表现更为严重,并且,在输注循环单核细胞后,症状可逆转。
总而言之,本研究结果表明SCD循环单核细胞可清除溶血损伤的血管内皮,促进HO-1表达上调、抑制VOC;循环单核细胞数量浮动会导致HO-1hi的循环单核细胞数量减少,从而导致SCD患者发生VOC。简言之,HO-1hi的循环单核细胞在VOC病理过程中发挥重要作用,或许可作为VOC的治疗靶点。
原始出处:
Yunfeng Liu,et al. HO-1hi Patrolling Monocytes Protect against Vaso-occlusion in Sickle Cell Disease. Blood 2018 :blood-2017-12-819870; doi: https://doi.org/10.1182/blood-2017-12-819870
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#血管闭塞#
26
学习了谢谢分享!!
25
#单核细胞#
16