JAHA:接受冠状动脉搭桥术的急性冠状动脉综合征患者血小板静止治疗
2021-02-19 MedSci原创 MedSci原创
该研究的结果支持血小板静止在降低需要冠状动脉搭桥手术的急性冠状动脉综合征患者的死亡率方面的作用。这表明,急性冠状动脉综合征患者,无论是否接受冠状动脉搭桥术,都应预先常规使用更有效的抗血小板治疗策略。
对于需要冠状动脉搭桥术的急性冠脉综合征患者,最佳的抗血小板策略尚未明确。然而更有效的抗血小板治疗方案容易导致围手术期出血。“血小板静止”是一个由来已久的概念,近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究假设通过“血小板静止”治疗获得的残余血小板抑制作用可以延缓冠脉搭桥的时间,并具有缺血保护作用。
研究人员通过荟萃分析,比较了分别接受了更有效的抗血小板抑制策略和不那么有效的血小板抑制策略的冠状动脉搭桥手术患者。该研究的主要结局是旁路手术后患者的全因死亡率。
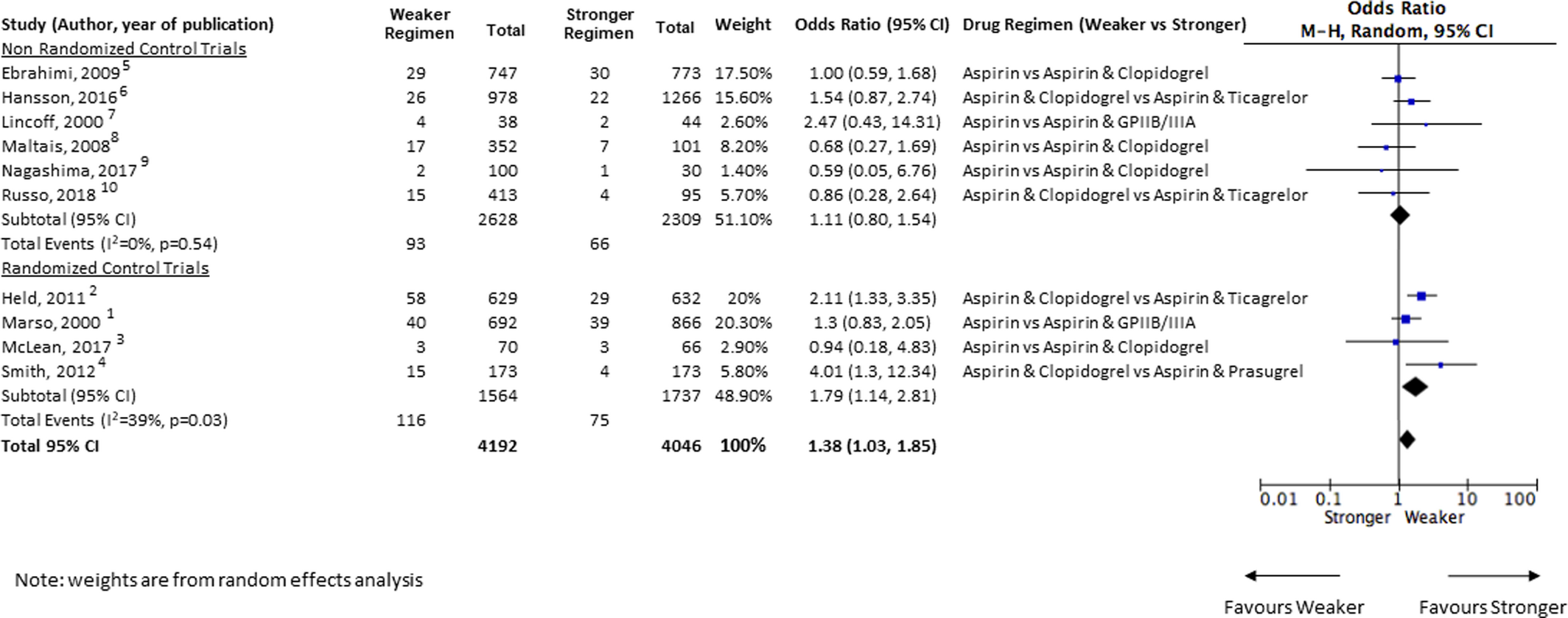
该荟萃分析确定了4项抗血小板治疗的随机化研究和6项非随机化研究。综合所有研究,接受不那么有效的血小板抑制策略的冠状动脉搭桥手术患者总体死亡率高于接受了更有效的抗血小板抑制策略的冠状动脉搭桥手术患者(比值比为1.38;95%置信区间为1.03-1.85;P=0.03)。
由此可见,该研究的结果支持血小板静止在降低需要冠状动脉搭桥手术的急性冠状动脉综合征患者的死亡率方面的作用。这表明,在急性冠状动脉综合征患者中,无论是否接受冠状动脉搭桥术,都应预先常规使用更有效的抗血小板治疗策略。
原始出处:
Kiran Sarathy.et al.Platelet Quiescence in Patients With Acute Coronary Syndrome Undergoing Coronary Artery Bypass Graft Surgery.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.016602
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#搭桥#
27
#冠状动脉综合征#
40
#AHA#
41
#综合征#
31
#搭桥术#
43
学习到了
79
好文
87