Cell Rep:重磅!癌症疫苗或许可行!《Cell》子刊揭肝癌疫苗!
2017-11-20 佚名 转化医学网
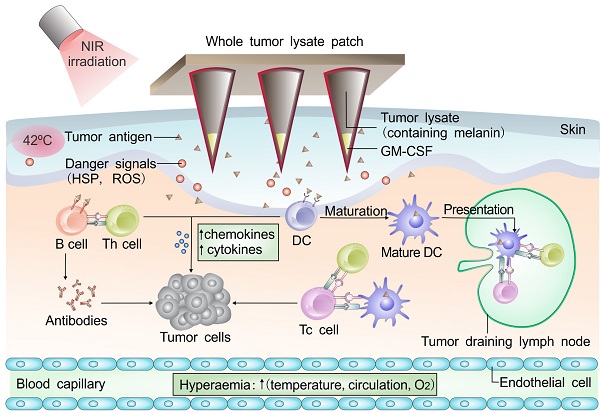
肝癌是导致癌症患者死亡的重要原因之一,其发病率和死亡率居高不下,全世界每年有78万新发肝癌患者和74万肝癌死亡病例。肝癌已成为除肺癌外第二致命的恶性肿瘤,在肝癌晚期,几乎没有十分有效的靶向药物或免疫治疗药物。可喜的是,近日发表在《Cell Report》上的一篇文章给我们带来了希望!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
25
#Cell#
28
#重磅#
24
叹为观止
72
签到学习了很多
71