International Journal of Nursing Studies:护士人力配置与住院患者死亡率之间的关系
2021-10-03 小文子 MedSci原创
注册护士人员配置水平与死亡率之间存在相关性,注册护士的级别越高,患者的预后越好。
几十年来,护理人力资源配置与患者预后之间的关系一直备受关注。护理人力资源配置与患者跌倒、医院感染和护理相关并发症有关。
发表在International Journal of Nursing Studies杂志的一篇文章,探索暴露于较低或较高级别注册护士/护理助理轮班时,患者的死亡率。
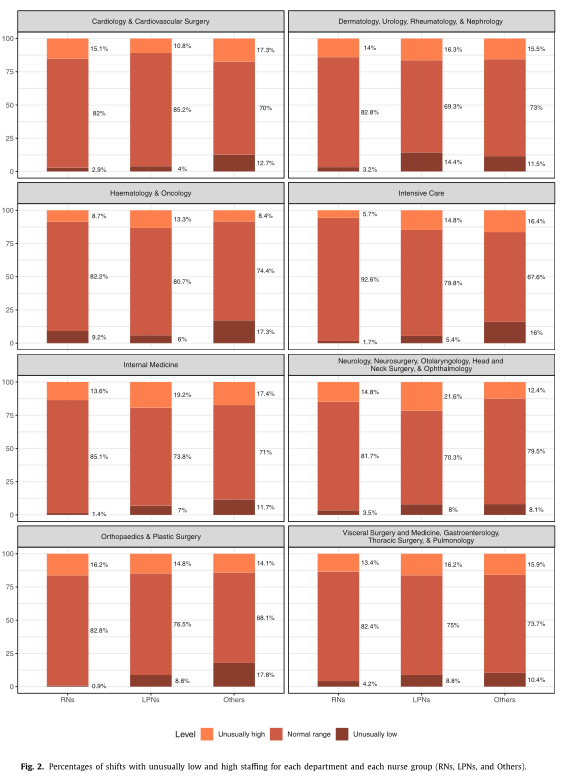
这项纵向研究使用瑞士一所大学医院三年(2015-2017年)的常规轮班、病房和患者水平数据。对55个病房、79893名成人住院患者和3646名护士(2670名注册护士、438名职业护士和538名助理护士和管理人员)的数据进行分析。开发人员配置模型确定高级别和低级别护士轮班后,研究人员拟合逻辑回归模型探索护士配置与死亡率之间的关系。
结果显示,暴露于高级别注册护士的轮班工作,患者死亡率降低8.7% [OR=0.91, 95%CI, 0.89-0.93]。相反,低级别注册护士轮班与10%的高死亡率相关[OR=1.10, 95%CI, 1.07–1.13]。其他群体人员轮班与死亡率之间的具体关系仍不清楚。例如,助理护士和管理人员的高级别和低级别配置均与较高死亡率相关,分别为1.03 [95%CI, 1.01–1.04]和1.04[95%CI, 1.03-1.06]。
患者水平的纵向研究表明,注册护士人员配置水平与死亡率之间存在相关性,注册护士的级别越高,患者的预后越好(即死亡率越低),而级别越低,患者的预后越差(即死亡率越高)。从这些结果来看,其他三组对患者的安全性尚不清楚。因此,不建议任何一组来替代注册护士。研究人员认为,迫切需要研究合理的护士配置方案。
原文出处:
Sarah N. Musya, Olga Endrich,et al, The association between nurse staffing and inpatient mortality: A
shift-level retrospective longitudinal study, 2021, International Journal of Nursing Studies, https://doi.org/10.1016/j.ijnurstu.2021.103950
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#eRNA#
54
#studies#
28
#Nat#
38
#患者死亡#
40
#DIE#
37
好
39
迫切需要研究合理的护士配置方案
42