AJRCCM:自身免疫是特发性肺动脉高压的一个重要特征
2022-03-26 刘少飞 MedSci原创
自身免疫被认为在特发性肺动脉高压 (IPAH) 中起作用。目前尚不清楚这是疾病的病因还是旁观者,以及它是否具有任何预后或治疗意义。
肺动脉高压 (PAH) 的特征是肺动脉严重重塑,导致肺血管阻力增加,导致心输出量减少、右心衰竭,尽管有许多许可疗法,但预期寿命缩短。 PAH 是一种混合的病理分类,公认的女性占优势,并且已知与女性流行的自身免疫性疾病相关,包括系统性硬化症-PAH (SSc-PAH)、系统性红斑狼疮 (SLE) 和干燥综合征。最常见的专科中心诊断仍然是特发性 PAH (IPAH),其原因仍未确定。 IPAH 患者表现出自身免疫性疾病的重叠特征,包括肺部炎症和免疫细胞浸润,以及推定的循环自身抗体。 IPAH 代表一种未确诊的自身免疫性疾病的概念已经流传了几十年。全基因组测序的可用性已经阐明,只有适度比例的 IPAH 患者可能被重新归类为具有罕见的致病突变,但增加了自身免疫假设的分量,来自常见遗传变异分析的主要信号位于一个 HLA 相关基因座和最近的全血转录组学无监督聚类确定了免疫球蛋白转录之间的差异作为 IPAH 患者生存良好和不良聚类的决定因素。无论自身免疫或炎症的因果与关联性质如何,它仍然是药物再利用的有吸引力的目标。迄今为止,还没有试验成功确定免疫调节剂疗法的反应者。有必要更好地了解 IPAH 中免疫失调患者的性质和比例,以指导病理生理学研究和未来的治疗试验。
本研究目的:
使用大型横断面队列研究 IPAH 中的自身免疫。
研究方法:
使用流式细胞术评估循环免疫细胞表型,并使用标准化的多重阵列生成血清免疫球蛋白谱,该阵列由 473 例病例和 946 例对照中的 19 种临床验证自身抗体组成。额外的 GST 融合阵列和 ELISA 数据用于鉴定针对 BMPR2 的血清自身抗体。聚类分析和临床相关性被用来确定免疫原性和临床结果之间的关联。
研究主要结果:
流式细胞免疫分析表明,除了 IgG3 升高外,IPAH 还与体液免疫反应的改变有关。多重自身抗体在 IPAH 中显着升高,并且聚类显示了三个不同的聚类:“高自身抗体”、“低自身抗体”和一个小“中间”聚类,表现出高水平的 RNP 复合物。高自身抗体簇的血流动力学较差,但存活率提高。一小部分患者表现出对 BMPR2 的免疫球蛋白反应性。
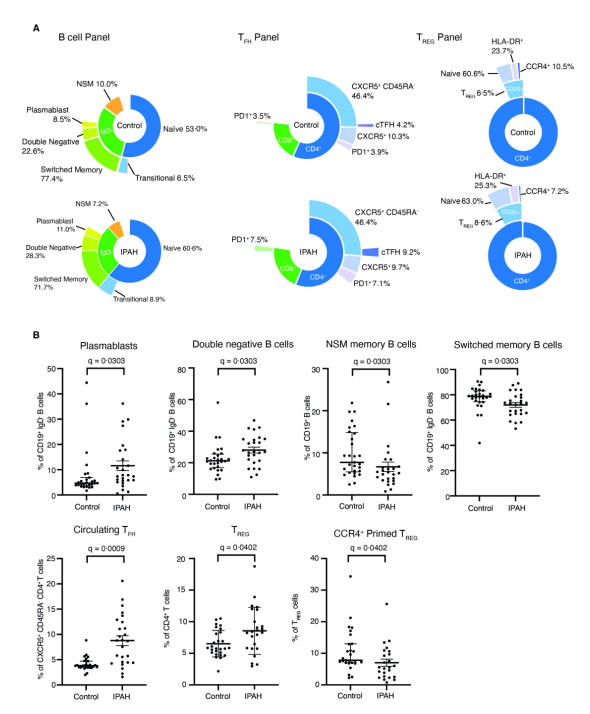
图1. IPAH的外周免疫谱是激活的免疫反应之一。
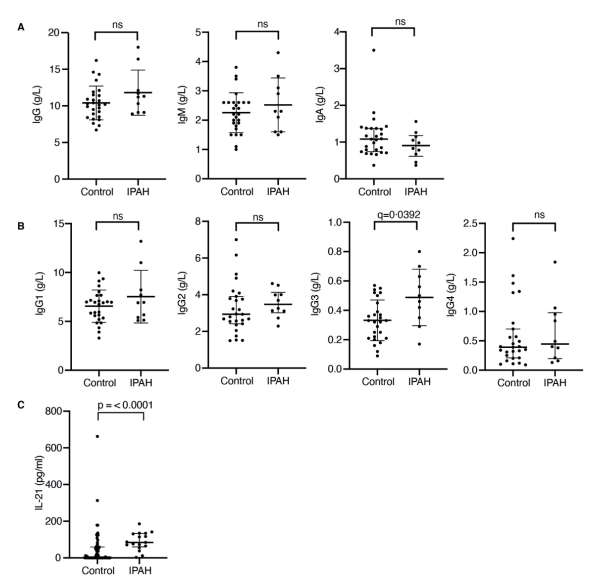
图2. IPAH的循环免疫球蛋白和白细胞介素-21水平。
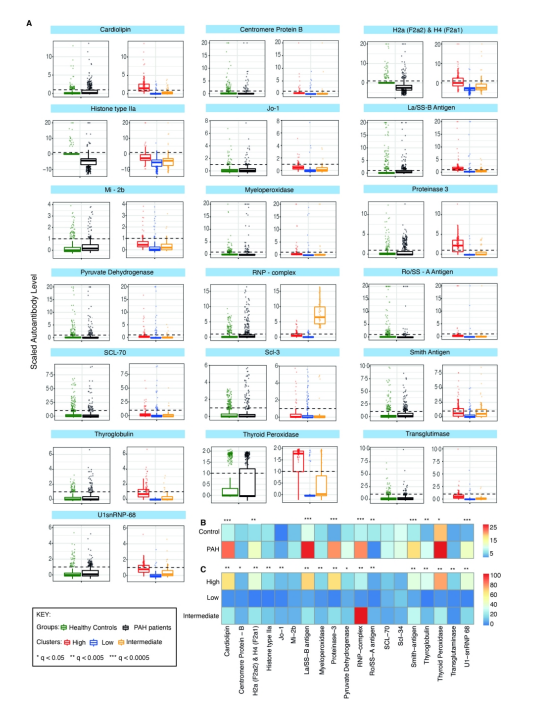
图3. PAH的自身抗体分析。
研究结论:
本研究将异常免疫调节和自身抗体的存在确定为大部分 IPAH 患者特征的关键特征,并且与临床结果相关。
参考文献:
Jones RJ, De Bie EMDD, Groves E, Zalewska KI, Swietlik EM, Treacy CM, Martin JM, Polwarth G, Li W, Guo J, Baxendale HE, Coleman S, Savinykh N, Coghlan JG, Corris PA, Howard LS, Johnson MK, Church C, Kiely DG, Lawrie A, Lordan JL, Mackenzie Ross RV, Pepke Zaba J, Wilkins MR, Wort SJ, Fiorillo E, Orrù V, Cucca F, Rhodes CJ, Gräf S, Morrell NW, McKinney EF, Wallace C, Toshner M; UK National PAH Cohort Study Consortium. Autoimmunity is a Significant Feature of Idiopathic Pulmonary Arterial Hypertension. Am J Respir Crit Care Med. 2022 Mar 22. doi: 10.1164/rccm.202108-1919OC. Epub ahead of print. PMID: 35316153.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#特发性#
35
#动脉高压#
41
#RCC#
44
#特发性肺动脉高压#
61
精彩评论,需要您登录查看
60