DOM:2型糖尿病患者早期和持续稳定的血糖控制与主要不良心血管事件(MACE)的减少相关
2022-04-25 从医路漫漫 MedSci原创
UKPDS的研究表明,即使在随后的血糖恶化之后,早期严格的血糖控制与大血管事件的减少有关。

背景:心血管疾病(CVD)是糖尿病患者死亡和残疾的主要原因,心血管疾病风险与较高的糖化血红蛋白(HbA1c)相关。UKPDS的研究表明,即使在随后的血糖恶化之后,早期严格的血糖控制与大血管事件的减少有关。2型糖尿病确诊后不久血糖控制与随后大血管事件的风险降低相关;而确诊后糖化血红蛋白模式恶化与长期合并症和死亡风险增加相关。这些发现导致了早期血糖控制的“遗留效应”(代谢记忆)的概念。支持遗传效应的机制尚未解决,但可能与表观遗传过程有关,如翻译后组蛋白甲基化的持续存在和葡萄糖正常化后microRNA的变化或阻止动脉壁中蛋白质基质的糖基化,从而抑制动脉粥样硬化病变的发展。
相反,只有在病程后期才严格控制血糖--在确诊为2型糖尿病数年之后--可能会导致不良的心血管后果。更大的血糖变异性被认为是一种病理生理机制。每日血糖值的波动或较长时间的波动(来访HbA1c)可能会导致氧化应激,促进炎症,内皮功能障碍,以及更多的大血管风险和死亡。2型糖尿病患者血糖变异性对血管预后的重要性受到挑战。目前尚不清楚,一旦血糖控制的早期阶段(与遗传效应有关)被考虑在内,血糖变异性是否会影响未来的大血管风险。到目前为止,很少有研究区分实现早期血糖控制所需的代谢流量与后期血糖变异性。
目的:旨在确定早期实现血糖控制以及随后的任何血糖变异性是否与重大不良心血管事件(MACE)风险的任何变化相关。
材料和方法:一项来自牛津-皇家全科医生研究和监督中心数据库的回溯性队列分析--一个大型的英国初级保健网络。我们在2005年1月1日或之后跟踪了新诊断的2型糖尿病患者,确诊时年龄≥为25岁,在确诊时和一年后都测量了糖化血红蛋白;之后又测量了≥5的糖化血红蛋白。A(HbA1c<58mmolm ol,7.5%)、B(HbA1c≥58~75mmoL/m ol,7.5~9.0%)和C(HbA1c≥75mmoL/m ol,9.0%)。从确诊到1年后,确定条带之间的移动。此外,对于前12个月后的数据,血糖变异性评分是根据连续的HbA1c读数相差0.5%(5.5mmoL/≥)计算的。使用时变的Cox比例风险模型评估诊断后1年发生MACE的风险,该模型包括第一年的转归和血糖变异性评分。
结果:26180例患者中有2300例发生MACE。与A->A组相比,C->A组患者发生MACE的危险性降低(HR0.75;95%CI为0.60~0.94;P=0.014),而C->C组患者的HR1.21(0.81~1.81;P=0.34)。与最低血糖变异性评分相比,最大变异性增加了MACE的风险(HR1.51;1.11-2.06;P=0.0096)。
表1 调整后的2型糖尿病患者MACE风险比

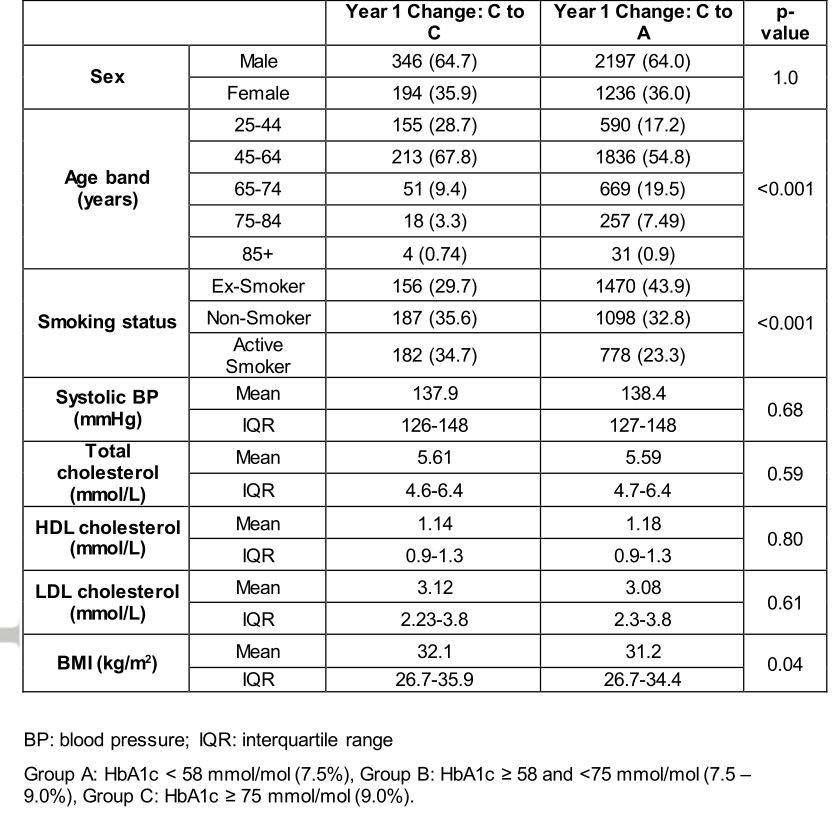
表2 保持HbA1c≥75 mmoL/m ol(9.0%)(C向C过渡)或从≥75 mmoL/m ol(9.0%)改变至HbA1c<58 mmoL/m ol(7.5%)(C至A过渡)超过12个月的人的特征
结论:早期控制糖化血红蛋白改善了2型糖尿病患者的心血管结局,尽管随后的血糖变化对个体仍有负面影响。
原文出处:Whyte MB, Joy M, Hinton W,et al.Early and ongoing stable glycaemic control is associated with a reduction in major adverse cardiovascular events in people with type 2 diabetes: A primary care cohort study.Diabetes Obes Metab 2022 Apr 04
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血管事件#
46
#ACE#
61
#MAC#
46
一直关注
57
以阅读
57
#血糖控制#
59
#2型糖尿病患者#
42
#糖尿病患者#
39
#主要不良心血管事件#
44
#MACE#
43