房颤导管消融并发症的识别与处理
2017-10-14 Ivy.K 医学界心血管频道
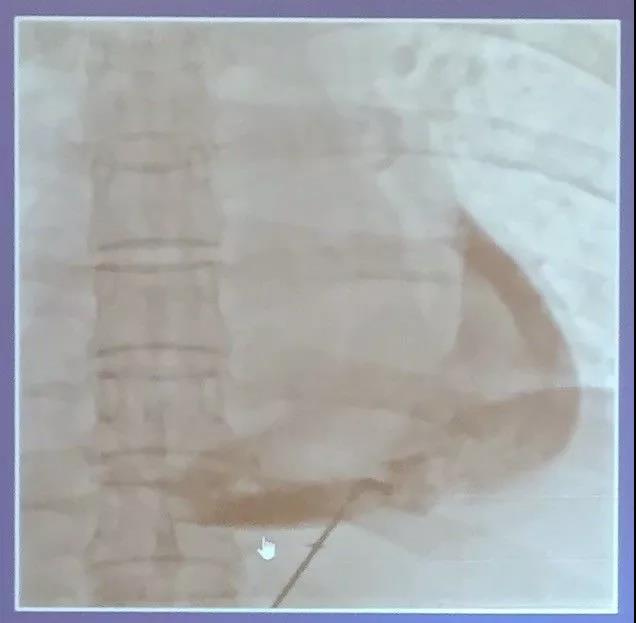
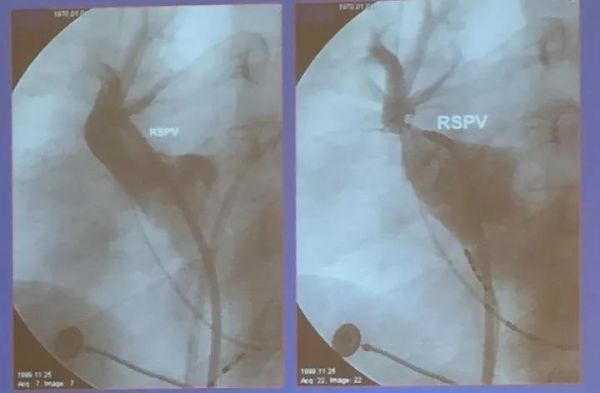
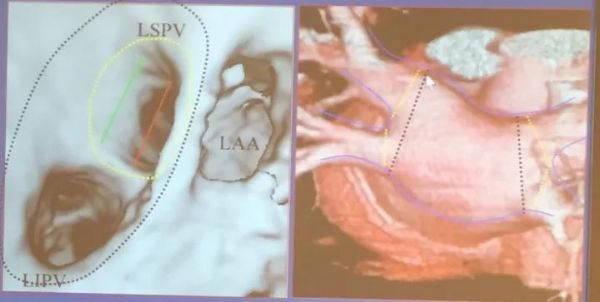
近年来,随着医疗技术的不断改善,房颤导管消融并发症呈下降趋势,2009年一项全球调查数据显示,房颤导管消融并发症的发生率为4.5%。 在第二十八届长城国际心脏病学会议中,来自首都医科大学附属北京朝阳医院的刘兴鹏教授带来了《房颤导管消融并发症的识别与处理》的精彩讲课,重点讲解了心肌穿孔/心脏压塞、肺静脉狭窄、脑卒中、心房食管瘘等房颤导管消融术的主要并发症,以下是小编整理的重点内容,分享给大家。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#并发#
29
#导管消融#
39
#消融#
39
还得加强自身学习
0
学习一下知识了谢谢
76
很好很好很好
86
学习了很有用
88
谢谢分享.学习了
87