JCI:新药Vorinostat使潜伏的HIV暴露更彻底,治疗取得重大进展!
2017-07-18 sunshine2015 来宝网
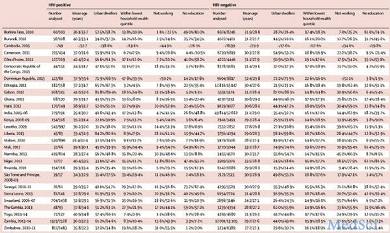
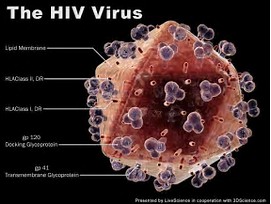
北卡罗来纳大学教堂山大学的研究人员已经表明,药物Vorinostat的间歇给药可以逆转艾滋病病毒,并且对艾滋病毒感染者的耐受性良好。然而,虽然Vorinostat使潜在的艾滋病毒易于检测,但它不能清除或消除感染,这意味着需要额外的进步来实现治愈。这些结果发表在7月17日的“临床调查杂志”上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#重大进展#
31
#JCI#
23
学习谢谢分享
63
学习了新知识
67
谢谢
53
很好,不错,以后会多学习
58