Eur J Cancer:HER2阳性早期可手术乳腺癌患者中,术前曲妥珠单抗联合依维莫司的疗效和预测标志物探索
2021-11-10 yd2015 MedSci原创
研究表明,依维莫司的加入并没有提高疗效,但诱导了MAPK信号通路。在这种情况下,应该考虑克服联合治疗导致的途径交叉,以使曲妥珠单抗的有效性最大化。
曲妥珠单抗在乳腺癌中的耐药性是一个持续的挑战。近期,European Journal of Cancer杂志发表一项II期研究 (RADHER),在 HER2阳性早期可手术乳腺癌患者中,术前曲妥珠单抗中加入mTOR抑制剂依维莫司的疗效和预测标志物探索。
患者随机1:1接受曲妥珠单抗(初始剂量4mg /kg,然后每周2mg /kg,持续5周)单独(T)或联合依维莫司(10 mg/天,持续6周)(T+E),然后进行手术。在基线和治疗时,通过临床检查和超声检查对肿瘤进行评估。主要终点为6周时的临床缓解率。病理反应和安全性也进行了评估。通过免疫组化和多重免疫分析评估基线和手术肿瘤样本,预测PI3K/AKT/mTOR和MAP激酶(MAPK)通路的下游效应因子的预测性。
2008年7月至2012年4月期间纳入82例患者,两组各41例患者。曲妥珠单抗单药(T)和曲妥珠单抗联合依维莫司(T+E)组的临床缓解率分别为34.1%和43.9%,病理缓解率分别为43.6%和47.5%。两组间无统计学差异。激素受体阳性(HR+)和激素受体阴性(HR-)患者的临床缓解率(P=0.82)和病理缓解率(P=0.36)没有观察到显著差异。
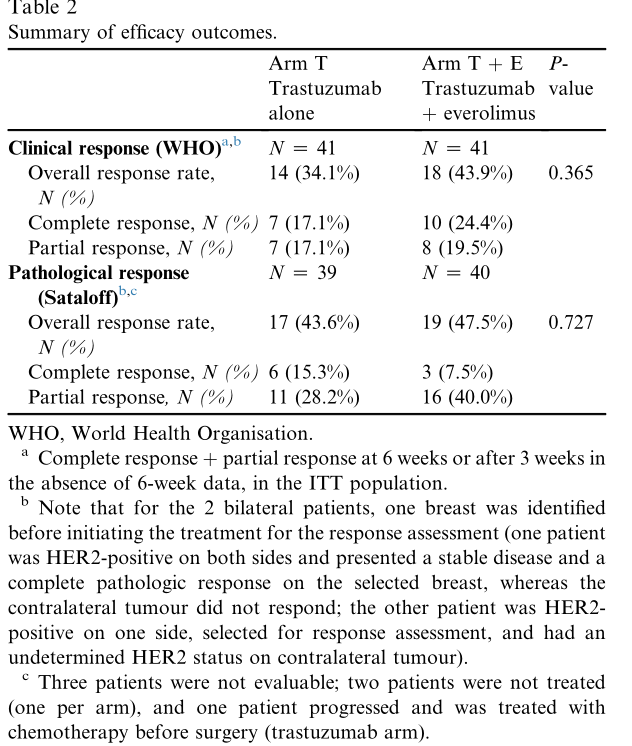
临床疗效
添加依维莫司可增加毒性,特别是粘膜炎(82.5% vs . 5.0%)和皮疹(57.5% vs . 10.0%),但III/IV级事件很少。T+E组的III-IV级AEs为 22.5%,明显较T组增加(p=0.002)。
两组Ki-67在基线和手术之间显著降低(P<0.001)。两组之间没有观察到差异。尽管在T组中,临床完全应答者和非完全应答者没有观察到差异,但T+ E组有显著差异(P =0.036)。caspase-3的表达水平均没有差异,也与应答无关。

标志物分析
考虑到整个患者群体,PIK3CA突变(P=0.991)和PTEN抑制率(P= 0.300)在基线和手术标本之间没有观察到显著变化。PIK3CA突变状态跟临床应答有关(P=0.029),PIK3CA野生型患者的ORR为92%,而PIK3CA突变患者的ORR为8%。
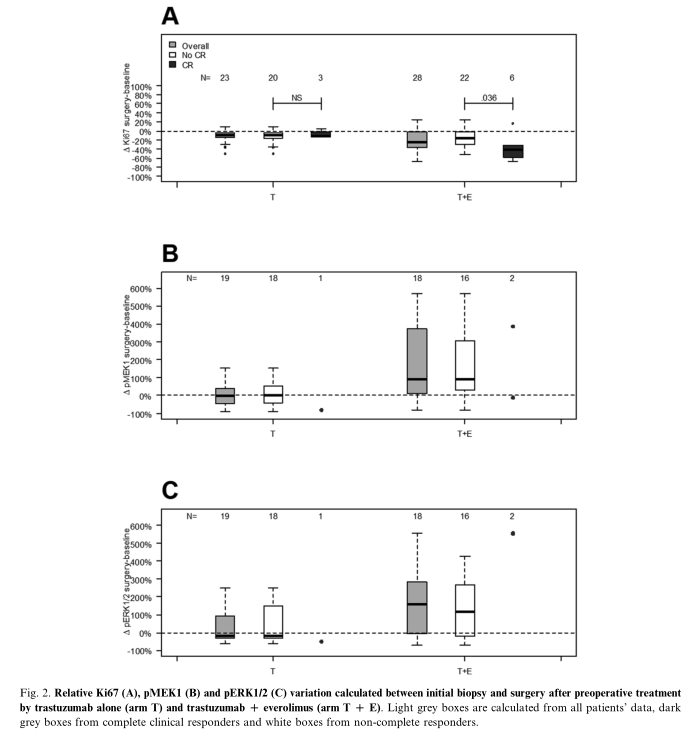
在T组中, pMEK1和pERK1/2在基线和手术之间没有明显差异。而在T+E组中, pMEK1 (P=0.005)和pERK1/2 (P= 0.030)观察到明显差异。因此,pMEK1和pERK1/2的表达水平在T和T+E组中有差异 (p分别为0.014和0.017)。
综上,研究表明,依维莫司的加入并没有提高疗效,但诱导了MAPK信号通路。在这种情况下,应该考虑克服联合治疗导致的途径交叉,以使曲妥珠单抗的有效性最大化。
原始出处:
Campone M, Bachelot T, Treilleux I, Pistilli B, Salleron J, Seegers V, Arnedos M, Loussouarn D, Wang Q, Vanlemmens L, Jimenez M, Rios M, Diéras V, Leroux A, Paintaud G, Rezai K, André F, Lion M, Merlin JL. A phase II randomised study of preoperative trastuzumab alone or combined with everolimus in patients with early HER2-positive breast cancer and predictive biomarkers (RADHER trial). Eur J Cancer. 2021 Oct 19;158:169-180. doi: 10.1016/j.ejca.2021.09.017. Epub ahead of print. PMID: 34678678.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#标志物#
25
#曲妥珠#
42
#HER2阳性#
47
#乳腺癌患者#
34