四个诊断腰椎管狭窄的MRI征象,千万不能忽视
2020-06-17 医护多团队 影像论坛
腰椎管狭窄症(LSS)是我国中老年人常见的退行性疾病。随着人口老龄化,其发病率也在大幅度增加。
腰椎管狭窄症(LSS)是我国中老年人常见的退行性疾病。随着人口老龄化,其发病率也在大幅度增加。
目前临床诊断腰椎管狭窄主要依据患者的症状、电生理学和影像学检查,而影像学上关于腰椎管狭窄诊断、分型和分级的参考指标很多,但都因为测量费时、复杂、可重复性低和个体差异等原因没有得到广泛使用。
不过在长期的实际工作中,我们发现一些特殊的影像学表现能够客观反映狭窄,对LSS的诊断具有重要的临床意义。
马尾神经冗余征
马尾神经的脊神经根在椎管内几乎垂直下行,围绕终丝聚集成束,形成马尾。生理状态下,马尾神经漂浮于脑脊液中,仰卧位时受重力作用,走形分布靠近背侧。
当人体站立或坐位时,在力学系统的传导影响下,腰椎间盘发生压缩、椎小关节紧张、关节间隙变窄等改变,此时腰椎管内压力增加,尤其是前屈位时。为抵抗和适应这种额外负荷的增加,机体会本能地做出调整,使得上述改变加大,相同层面的椎管容积缩小;当人体卧位时,重力系统的传导消失,负荷解除,椎管容积将最大限度恢复。
然而,当腰椎管狭窄到一定程度时,硬膜囊受压变窄,卡压其内的马尾神经,限制其正常活动。当腰椎屈曲时,马尾神经受到牵拉,通过狭窄处上移,等到腰椎恢复到直立位或后伸时,马尾神经通过自身的解剖维系结构则难以复位,于是在狭窄水平以上出现环状、迂曲、松弛、缠绕等现象,这时就是我们所说的马尾神经冗余征。
据相关文献报道,年龄、腰椎管多节段狭窄、狭窄层面硬膜囊面积、腰椎管狭窄的位置、狭窄处锐利突起等是其危险因素。不过,也有少数腰椎管狭窄患者不会出现这种征象,比如年轻、单椎管狭窄、椎管先天发育宽大的患者。

图1 患者,女,76岁,腰腿疼多年伴偶发神经源性跛行
A:MRI矢状位示腰椎体上缘至腰4/5椎间盘区间,可见腰椎管多节段狭窄及椎管内马尾神经迂曲冗长
B:MRI轴位示增粗的马尾神经在狭窄内的异常分布排列

图2 患者,女,54岁,双下肢交替出现疼痛无力麻木多年
A:MRI矢状位示腰1椎体上缘至腰4/5水平段,显示腰椎间盘多发突出及腰椎管多节段狭窄,狭窄椎管内的马尾神经迂曲冗长
B:MRI轴位示马尾神经的正常结构消失,形态增粗,分布成团,排列紊乱
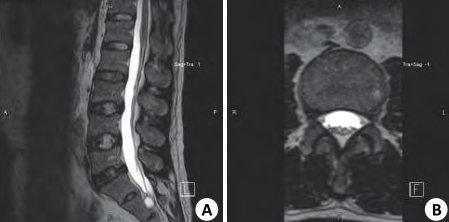
图3 25岁男性志愿者
A:MRI矢状位示正常椎管及其椎管内分布排列的马尾神经根,腰1至腰5椎体上缘马尾神经均靠背侧整束行走,形态自然
B:MRI轴位示马尾神经分布在椎管后1/3份,粗细均匀,排列规整
马尾神经沉降征
马尾神经沉降征是腰椎管狭窄的另一个MRI表现。上面我们提到过,正常情况下马尾神经漂浮在脑脊液中,仰卧位时分布在椎管背侧。如果患者仰卧位时,其马尾神经仍漂浮在脑脊液中,就可以定义为沉降征阳性。
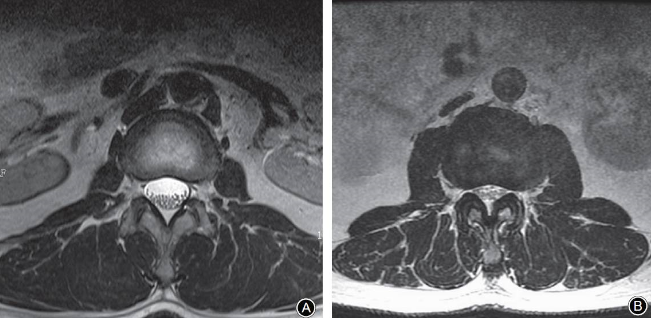
图4 马尾神经沉降征的阴性和阳性表现
A:患者,女,56岁,体格检查健康,无明显腰部和下肢不适,腰椎MRI横断面T2W1图像显示神经根都位于椎管的背侧,表现为马尾神经沉降征阴性
B:患者,女,65岁,间歇性跛行1年余,MRI横断面T2W1图像显示椎管狭窄,黄韧带肥厚,马尾神经悬浮于椎管内,部分神经根位于椎管腹侧,表现为马尾神经沉降征阳性
另外,有研究证实,在L5平面以上症状和影像学符合中央椎管狭窄的患者中,沉降征的阳性率为94%;而没有椎管狭窄症状的腰痛患者中,其发生率几乎为零。这也就说明,马尾神经沉降征的另一个重要意义在于,可以作为区分单纯下腰痛和腰椎管狭窄的特征性指标。
前方脑脊液空间闭塞
2011年,有学者提出通过脑脊液前方空间的大小来评估腰椎管狭窄的严重程度,认为通过观测脑脊液前方空间的闭塞程度,便能了解椎管狭窄的严重程度。并且基于马尾神经和硬膜囊剩余脑脊液空间的相对比率,由马尾神经的分离程度决定分级:
0级:前方脑脊液空间无闭塞,马尾神经彼此界限清晰,无椎管狭窄;
1级:轻度椎管狭窄,前方脑脊液空间轻度闭塞,但马尾神经之间能清楚地辨别;
2级:中度椎管狭窄,前方脑脊液空间中度闭塞,部分马尾神经相互聚集,无法区分;
3级:严重椎管狭窄,前方脑脊液空间完全闭塞,硬膜囊显着受压,马尾神经未能清楚显示而表现为一束。
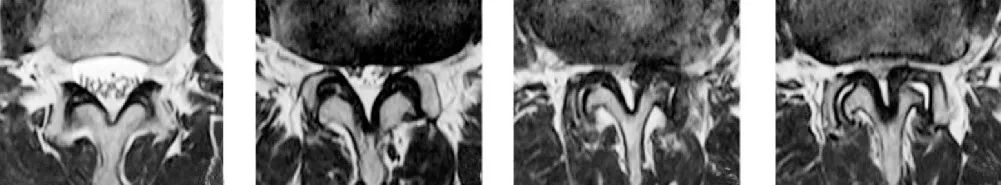
图5 前方脑脊液空间闭塞程度分级
(从左到右:0级、1级、2级、3级)
研究证实,前方脑脊液空间的闭塞程度与椎管狭窄患者的硬膜囊前后径和面积存在不同程度的相关性。尤其在L3-4和L4-5水平,无论是硬膜囊的前后径还是面积,各个分级之间都存在显着性差异。因此,观察前方脑脊液空间的闭塞程度可以客观反映椎管狭窄的严重程度。
硬膜外脂肪增多
在腰椎管狭窄的影像诊断中,除了主观的椎管大小评估,常用的还有椎管的前后径、面积、硬膜囊面积、关节突关节水平的黄韧带之间距离等定量指标,其中椎管的前后径和硬膜囊面积最常用。
我们通常将椎管前后径<1cm和硬膜囊面积<100mm2作为腰椎管狭窄的诊断标准。
但是,临床上有这样一类患者,他们的骨性椎管空间,无论是直径还是面积都在正常范围内,但测量的硬膜囊面积却明显小于正常值。
这类患者往往是由于椎管内占位导致的相对狭窄,而引起的硬膜囊受压。除了常见的肿瘤和血肿等占位因素,还有硬膜外正常的脂肪组织过度增生而导致的椎管狭窄,但由于脂肪作为「正常」组织往往被我们所忽略。

图5 患者,男,60岁,双下肢间歇性跛行3年余,加重半年
A:MRI正中矢状位T1W1图像显示硬膜外脂肪组织明显增多,尤其是L4-5椎间隙水平
B:L4-5椎间隙水平骨性椎管未见明显狭窄,但测量硬膜囊面积仅约55mm2,明显小于腰椎管狭窄的诊断标准
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#椎管#
57
#椎管狭窄#
46
#腰椎#
30
#腰椎管狭窄#
36
#腰椎管#
31