Sci Transl Med:癌症治疗新可能:针对“僵硬”肿瘤的生物物理大杀器
2017-07-31 佚名 转化医学网
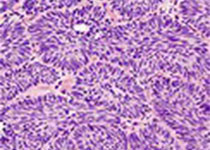
加州大学尔湾分校科学家Weian Zhao博士实验室通过基因工程建立了一种新的间充质干细胞(MSC),这种新型干细胞可以靶向识别“僵硬”的转移性肿瘤细胞,并将癌症药物精准递送至肿瘤组织。
Liu L, Zhang SX, Liao W,et al.Mechanoresponsive stem cells to target cancer metastases through biophysical cues.Sci Transl Med. 2017 Jul 26;9(400). pii: eaan2966. doi: 10.1126/scitranslmed.aan2966.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#癌症治疗#
29
#Transl#
28
#TRA#
26
#Med#
23
学习了,谢谢
57